Blog
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 473
[blogcat_id] => 5
[blog_title] => Importance Of Nutrition in Fertility
[metaTitle] => Understanding How Nutrition Plays a Key Role in Fertility
[metaDescription] => Discover the crucial role nutrition plays in fertility and learn key tips for improving your chances of conception.
[metaKeywords] =>
[seo_url] => importance-of-nutrition-in-fertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1711501682importance of nutrition in fertility.webp
[blog_text] => In today's day and age, many couples face challenges when trying to conceive. Infertility affects both men and women, and it can be a frustrating and emotional journey. While there are various medical treatments available, one aspect that often gets overlooked is the role of nutrition in fertility. A healthy diet plays a vital role in optimising reproductive health and increasing the chances of conception. Let's explore why nutrition is so important for fertility and what you can do to enhance your chances of getting pregnant.
Why is Nutrition Important for Fertility?
Nutrition plays a vital role in reproductive health for both men and women. It affects hormone production, egg quality, sperm count and overall reproductive function. A well-balanced diet can optimise your fertility by providing essential nutrients that support the reproductive system.
1. Achieving a healthy weight:
Maintaining a healthy weight is crucial for fertility. Being underweight or overweight can negatively impact hormonal balance, ovulation, and sperm production. Women who are underweight may experience irregular menstrual cycles or even stop ovulating altogether. On the other hand, obesity can cause insulin resistance, leading to hormonal imbalances and reduced sperm quality in men.
2. Enhancing egg quality:
For women, the quality of eggs is directly related to their ability to conceive naturally or through assisted reproductive techniques like IVF procedure or IUI treatment. A diet rich in antioxidants, vitamins (especially folate), minerals (such as zinc and selenium) and omega-3 fatty acids can help improve egg quality. Include fertility foods like leafy greens, citrus fruits, nuts, seeds, oily fish and whole grains to optimise your nutrient intake.
3. Boosting sperm health:
For men, proper nutrition is essential for optimal sperm production and function. Nutrients like zinc, folic acid, vitamin C, vitamin E, selenium and omega-3 fatty acids are known to support sperm health. Incorporate fertility foods like oysters, spinach, citrus fruits, berries, nuts, seeds, and fatty fish into your diet to enhance sperm count and motility.
Key Tips for a Healthy Conception
1. Eat a balanced diet:
Focus on consuming a well-balanced diet that includes whole grains, lean proteins, fruits, vegetables and healthy fats. Avoid processed foods, sugary snacks and excessive caffeine intake. Opt for organic and locally sourced produce whenever possible to reduce exposure to harmful pesticides.
2. Stay hydrated:
Proper hydration is crucial for overall health and fertility. Drink an adequate amount of water throughout the day to keep your body hydrated and support optimal reproductive function.
3. Include fertility foods:
Incorporate fertility foods into your daily meals. Some examples include:
- Leafy greens: Spinach, kale and broccoli are rich in folate and other essential nutrients.
- Berries: Blueberries, strawberries and raspberries are packed with antioxidants that protect against oxidative stress.
- Citrus fruits: Oranges, lemons and grapefruits provide vitamin C and folic acid.
- Nuts and seeds: Almonds, walnuts, flaxseeds and chia seeds are excellent sources of healthy fats and essential minerals.
- Colorful vegetables: Carrots, bell peppers, sweet potatoes and tomatoes contain beneficial antioxidants.
4. Limit alcohol consumption:
Excessive alcohol consumption could result in both female and male infertility issues. It can disrupt hormone levels in women and reduce sperm quality in men. If you're trying to conceive, it's best to limit your alcohol intake or avoid it altogether.
5. Manage stress levels:
Stress can interfere with regular ovulation in women and affect sperm production in men. Incorporate stress-reducing activities into your daily routine such as yoga, meditation or regular exercise to promote a healthy reproductive system.
In conclusion, nutrition plays a crucial role in fertility. By adopting a well-balanced diet that includes fertility foods and maintaining a healthy weight, you can optimise your chances of conceiving. Remember to consult with a fertility specialist for personalised advice and guidance on your journey to parenthood.
To learn more about the role of nutrition in fertility and explore personalised treatment options, schedule a consultation with expert fertility doctors at Apollo Fertility today.
FAQs
Q1: Can nutrition alone solve fertility issues?
A1: While proper nutrition plays a significant role in fertility, it may not be the sole solution for everyone. If you're struggling with infertility, it's essential to consult with a fertility specialist who can assess your specific situation and recommend appropriate treatments or interventions.
Q2: How long does it take for changes in nutrition to affect fertility?
A2: The impact of dietary changes on fertility can vary from person to person. It generally takes a few months for nutritional improvements to positively affect reproductive health. Be patient and consistent with your dietary choices.
Q3: Are there any specific foods to avoid when trying to conceive?
A3: It is advisable to limit your intake of processed foods, sugary snacks, trans fats and excessive caffeine. These foods can negatively impact fertility and overall health.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6568019/
https://www.sciencedirect.com/science/article/pii/S2161831322005129
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-27 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-27 01:08:02 [updatedDate] => 2024-03-27 01:10:54 [ip_address] => 49.205.116.233 ) [_oldAttributes:yii\db\BaseActiveRecord:private] => Array ( [blog_id] => 473 [blogcat_id] => 5 [blog_title] => Importance Of Nutrition in Fertility [metaTitle] => Understanding How Nutrition Plays a Key Role in Fertility [metaDescription] => Discover the crucial role nutrition plays in fertility and learn key tips for improving your chances of conception. [metaKeywords] => [seo_url] => importance-of-nutrition-in-fertility [city_id] => [city_name] => [language_id] => 1 [blog_image] => blog-images/1711501682importance of nutrition in fertility.webp [blog_text] =>In today's day and age, many couples face challenges when trying to conceive. Infertility affects both men and women, and it can be a frustrating and emotional journey. While there are various medical treatments available, one aspect that often gets overlooked is the role of nutrition in fertility. A healthy diet plays a vital role in optimising reproductive health and increasing the chances of conception. Let's explore why nutrition is so important for fertility and what you can do to enhance your chances of getting pregnant.
Why is Nutrition Important for Fertility?
Nutrition plays a vital role in reproductive health for both men and women. It affects hormone production, egg quality, sperm count and overall reproductive function. A well-balanced diet can optimise your fertility by providing essential nutrients that support the reproductive system.
1. Achieving a healthy weight:
Maintaining a healthy weight is crucial for fertility. Being underweight or overweight can negatively impact hormonal balance, ovulation, and sperm production. Women who are underweight may experience irregular menstrual cycles or even stop ovulating altogether. On the other hand, obesity can cause insulin resistance, leading to hormonal imbalances and reduced sperm quality in men.
2. Enhancing egg quality:
For women, the quality of eggs is directly related to their ability to conceive naturally or through assisted reproductive techniques like IVF procedure or IUI treatment. A diet rich in antioxidants, vitamins (especially folate), minerals (such as zinc and selenium) and omega-3 fatty acids can help improve egg quality. Include fertility foods like leafy greens, citrus fruits, nuts, seeds, oily fish and whole grains to optimise your nutrient intake.
3. Boosting sperm health:
For men, proper nutrition is essential for optimal sperm production and function. Nutrients like zinc, folic acid, vitamin C, vitamin E, selenium and omega-3 fatty acids are known to support sperm health. Incorporate fertility foods like oysters, spinach, citrus fruits, berries, nuts, seeds, and fatty fish into your diet to enhance sperm count and motility.
Key Tips for a Healthy Conception
1. Eat a balanced diet:
Focus on consuming a well-balanced diet that includes whole grains, lean proteins, fruits, vegetables and healthy fats. Avoid processed foods, sugary snacks and excessive caffeine intake. Opt for organic and locally sourced produce whenever possible to reduce exposure to harmful pesticides.
2. Stay hydrated:
Proper hydration is crucial for overall health and fertility. Drink an adequate amount of water throughout the day to keep your body hydrated and support optimal reproductive function.
3. Include fertility foods:
Incorporate fertility foods into your daily meals. Some examples include:
- Leafy greens: Spinach, kale and broccoli are rich in folate and other essential nutrients.
- Berries: Blueberries, strawberries and raspberries are packed with antioxidants that protect against oxidative stress.
- Citrus fruits: Oranges, lemons and grapefruits provide vitamin C and folic acid.
- Nuts and seeds: Almonds, walnuts, flaxseeds and chia seeds are excellent sources of healthy fats and essential minerals.
- Colorful vegetables: Carrots, bell peppers, sweet potatoes and tomatoes contain beneficial antioxidants.
4. Limit alcohol consumption:
Excessive alcohol consumption could result in both female and male infertility issues. It can disrupt hormone levels in women and reduce sperm quality in men. If you're trying to conceive, it's best to limit your alcohol intake or avoid it altogether.
5. Manage stress levels:
Stress can interfere with regular ovulation in women and affect sperm production in men. Incorporate stress-reducing activities into your daily routine such as yoga, meditation or regular exercise to promote a healthy reproductive system.
In conclusion, nutrition plays a crucial role in fertility. By adopting a well-balanced diet that includes fertility foods and maintaining a healthy weight, you can optimise your chances of conceiving. Remember to consult with a fertility specialist for personalised advice and guidance on your journey to parenthood.
To learn more about the role of nutrition in fertility and explore personalised treatment options, schedule a consultation with expert fertility doctors at Apollo Fertility today.
FAQs
Q1: Can nutrition alone solve fertility issues?
A1: While proper nutrition plays a significant role in fertility, it may not be the sole solution for everyone. If you're struggling with infertility, it's essential to consult with a fertility specialist who can assess your specific situation and recommend appropriate treatments or interventions.
Q2: How long does it take for changes in nutrition to affect fertility?
A2: The impact of dietary changes on fertility can vary from person to person. It generally takes a few months for nutritional improvements to positively affect reproductive health. Be patient and consistent with your dietary choices.
Q3: Are there any specific foods to avoid when trying to conceive?
A3: It is advisable to limit your intake of processed foods, sugary snacks, trans fats and excessive caffeine. These foods can negatively impact fertility and overall health.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6568019/
https://www.sciencedirect.com/science/article/pii/S2161831322005129
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-27 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-27 01:08:02 [updatedDate] => 2024-03-27 01:10:54 [ip_address] => 49.205.116.233 ) [_related:yii\db\BaseActiveRecord:private] => Array ( ) [_relationsDependencies:yii\db\BaseActiveRecord:private] => Array ( ) [_errors:yii\base\Model:private] => [_validators:yii\base\Model:private] => [_scenario:yii\base\Model:private] => default [_events:yii\base\Component:private] => Array ( ) [_eventWildcards:yii\base\Component:private] => Array ( ) [_behaviors:yii\base\Component:private] => Array ( ) )
Importance Of Nutrition in Fertility
March 27, 2024In today's day and age, many couples face challenges when trying t...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 472
[blogcat_id] => 8
[blog_title] => Assisted Reproductive Technology: Definition, Benefits
[metaTitle] => What Is Assisted Reproductive Technology?
[metaDescription] => Understand what is assisted reproductive technology (ART) and its benefits for couples facing fertility challenges.
[metaKeywords] =>
[seo_url] => assisted-reproductive-technology-definition-benefits
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1711170362assisted-reproductive-technology-definition-benefits.webp
[blog_text] => Struggling to conceive can be emotionally challenging for couples. Fortunately, advancements in medical science have paved the way for treatments that can help overcome infertility issues. One such solution is Assisted Reproductive Technology (ART), a range of procedures and treatments designed to assist individuals and couples in achieving pregnancy. In this blog, we will explore the definition of ART and its benefits, providing you with valuable information to make informed decisions about your fertility journey.
What is ART?
ART refers to medical interventions that support conception by handling eggs, sperm or embryos outside of the body. These procedures are performed in a controlled laboratory setting and can include techniques such as in vitro fertilisation or IVF procedure, intrauterine insemination or IUI treatment and fertility preservation.
IVF procedure involves the retrieval of eggs from a woman's ovaries, which are then fertilised with sperm in a laboratory. The resulting embryos are then transferred back into the uterus to establish pregnancy. IUI treatment, on the other hand, involves placing washed and prepared sperm directly into a woman's uterus during her ovulation period to increase the chances of fertilisation.
Benefits of ART
- Increased Pregnancy Success Rates: ART has revolutionised modern medicine by significantly improving pregnancy success rates for individuals and couples struggling with infertility issues. With advancements in laboratory techniques and protocols, ART offers hope to those who may have previously believed that conceiving a child was impossible.
- Tailored Treatment Plans: Each person's fertility journey is unique. By evaluating both female and male infertility factors, fertility specialists can develop personalised treatment plans to address specific concerns with the help of ART.
- Addressing Male Infertility: ART is not limited to addressing female infertility alone. It also offers solutions for couples facing male infertility issues. Through procedures such as Intracytoplasmic Sperm Injection (ICSI), which involves injecting a single sperm into an egg, even severe cases of male infertility can be overcome.
- Fertility Preservation: ART also allows individuals and couples to preserve their fertility for future use. Those undergoing medical treatments that could potentially affect their reproductive health, such as chemotherapy or radiation therapy, can opt for options like egg or sperm freezing. This preserves their ability to conceive in the future when they are ready.
- Supportive Care: Apart from the medical aspect, fertility clinics offering ART also provide emotional and psychological support throughout the treatment process. The compassionate and empathetic approach of fertility doctors helps patients navigate the highs and lows of their fertility journey with understanding and guidance.
In conclusion, ART offers hope and solutions to individuals and couples facing fertility challenges. With its personalised approach and advanced techniques, ART has transformed the lives of many by helping them realise their dream of parenthood. If you are ready to take the next step in your fertility journey, we encourage you to reach out to Apollo Fertility for expert guidance and support.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-23
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-23 05:06:02
[updatedDate] => 2024-03-23 05:06:02
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 472
[blogcat_id] => 8
[blog_title] => Assisted Reproductive Technology: Definition, Benefits
[metaTitle] => What Is Assisted Reproductive Technology?
[metaDescription] => Understand what is assisted reproductive technology (ART) and its benefits for couples facing fertility challenges.
[metaKeywords] =>
[seo_url] => assisted-reproductive-technology-definition-benefits
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1711170362assisted-reproductive-technology-definition-benefits.webp
[blog_text] => Struggling to conceive can be emotionally challenging for couples. Fortunately, advancements in medical science have paved the way for treatments that can help overcome infertility issues. One such solution is Assisted Reproductive Technology (ART), a range of procedures and treatments designed to assist individuals and couples in achieving pregnancy. In this blog, we will explore the definition of ART and its benefits, providing you with valuable information to make informed decisions about your fertility journey.
What is ART?
ART refers to medical interventions that support conception by handling eggs, sperm or embryos outside of the body. These procedures are performed in a controlled laboratory setting and can include techniques such as in vitro fertilisation or IVF procedure, intrauterine insemination or IUI treatment and fertility preservation.
IVF procedure involves the retrieval of eggs from a woman's ovaries, which are then fertilised with sperm in a laboratory. The resulting embryos are then transferred back into the uterus to establish pregnancy. IUI treatment, on the other hand, involves placing washed and prepared sperm directly into a woman's uterus during her ovulation period to increase the chances of fertilisation.
Benefits of ART
- Increased Pregnancy Success Rates: ART has revolutionised modern medicine by significantly improving pregnancy success rates for individuals and couples struggling with infertility issues. With advancements in laboratory techniques and protocols, ART offers hope to those who may have previously believed that conceiving a child was impossible.
- Tailored Treatment Plans: Each person's fertility journey is unique. By evaluating both female and male infertility factors, fertility specialists can develop personalised treatment plans to address specific concerns with the help of ART.
- Addressing Male Infertility: ART is not limited to addressing female infertility alone. It also offers solutions for couples facing male infertility issues. Through procedures such as Intracytoplasmic Sperm Injection (ICSI), which involves injecting a single sperm into an egg, even severe cases of male infertility can be overcome.
- Fertility Preservation: ART also allows individuals and couples to preserve their fertility for future use. Those undergoing medical treatments that could potentially affect their reproductive health, such as chemotherapy or radiation therapy, can opt for options like egg or sperm freezing. This preserves their ability to conceive in the future when they are ready.
- Supportive Care: Apart from the medical aspect, fertility clinics offering ART also provide emotional and psychological support throughout the treatment process. The compassionate and empathetic approach of fertility doctors helps patients navigate the highs and lows of their fertility journey with understanding and guidance.
In conclusion, ART offers hope and solutions to individuals and couples facing fertility challenges. With its personalised approach and advanced techniques, ART has transformed the lives of many by helping them realise their dream of parenthood. If you are ready to take the next step in your fertility journey, we encourage you to reach out to Apollo Fertility for expert guidance and support.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-23
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-23 05:06:02
[updatedDate] => 2024-03-23 05:06:02
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

Assisted Reproductive Technology: Definition, Benefits
March 23, 2024Struggling to conceive can be emotionally challenging for couples. For...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 471
[blogcat_id] => 8
[blog_title] => How To Confirm Whether Sperm Went Inside
[metaTitle] => Confirming Sperm Penetration: Effective Methods and Techniques
[metaDescription] => Unsure how to determine if sperm has fertilised an egg? Read on to understand if sperm has been successfully deposited during intercourse or fertility treatments.
[metaKeywords] =>
[seo_url] => how-to-confirm-whether-sperm-went-inside
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1711089062how-to-confirm-whether-sperm-went-inside.webp
[blog_text] => When it comes to conceiving, couples often have questions or concerns about whether sperm has successfully fertilised an egg. This uncertainty can arise from various factors, including difficulties with natural conception or undergoing fertility treatments like IVF procedure (In Vitro Fertilisation) or IUI procedure (Intrauterine Insemination). Understanding how to confirm whether sperm went inside can help alleviate some of the anxiety and provide guidance for those on their fertility journey.
The Importance of Confirming Sperm Deposition
Confirming whether sperm has gone inside is crucial for assessing fertility potential and determining the effectiveness of assisted reproductive techniques, like IVF procedure or IUI treatment. It allows couples and fertility doctors to make informed decisions regarding future treatment plans and interventions.
Methods to Confirm Sperm Deposition
There are several methods to confirm whether sperm has successfully reached the cervix or uterus:
1) Basal Body Temperature (BBT) Tracking:
Monitoring your BBT can provide insights into your menstrual cycle and potential ovulation. This can be done using a special BBT thermometer. After ovulation, if fertilisation occurs, the BBT remains elevated due to increased progesterone levels.
2) Cervical Mucus Monitoring:
Cervical mucus changes throughout the menstrual cycle, becoming thin and stretchy around ovulation. This fertile cervical mucus helps facilitate sperm movement towards the uterus.
3) Home Ovulation Test Kits:
These kits detect luteinising hormone (LH) levels in urine, indicating an impending ovulation. Having intercourse during this fertile window increases the chances of successful sperm deposition.
4) Post-Coital Test:
Also known as the Huhner test, this examination involves collecting a sample of cervical mucus within 2-24 hours after intercourse and assessing its quality and the presence of live, motile sperm. Post-coital tests can be scheduled at a fertility clinic near you.
4) Transvaginal Ultrasound:
A transvaginal ultrasound can provide visual confirmation of sperm deposition. It allows fertility specialists to visualise the cervix, uterus and fallopian tubes to ensure proper placement during fertility procedures.
Fertility Treatments and Confirmation
1) IVF procedure:
In the IVF procedure, the fertilisation process occurs outside the body. The sperm is directly introduced to the egg in a laboratory setting. Confirmation of successful fertilisation is determined by observing embryo development after insemination.
2) IUI treatment:
During the IUI treatment, prepared sperm is inserted into the uterus using a catheter. Confirming whether sperm has fertilised an egg is essential in assessing the success of the procedure. A post-IUI ultrasound may be performed to evaluate proper catheter placement.
Confirming whether sperm has gone inside is an important aspect of the fertility journey. Various methods, including BBT tracking, cervical mucus monitoring, home ovulation test kits, post-coital tests and ultrasounds, can help determine successful sperm deposition. If you have concerns or questions about your fertility, it's recommended to consult with a fertility specialist or healthcare professional who can guide you through the process and provide personalised recommendations.
At Apollo Fertility, we are here to support you on your fertility journey. Our experienced team of doctors and state-of-the-art facilities are dedicated to providing compassionate care and personalised treatment plans. Visit our website or schedule a consultation today to take the next step towards building your family.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-22
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-22 06:31:02
[updatedDate] => 2024-03-22 06:31:02
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 471
[blogcat_id] => 8
[blog_title] => How To Confirm Whether Sperm Went Inside
[metaTitle] => Confirming Sperm Penetration: Effective Methods and Techniques
[metaDescription] => Unsure how to determine if sperm has fertilised an egg? Read on to understand if sperm has been successfully deposited during intercourse or fertility treatments.
[metaKeywords] =>
[seo_url] => how-to-confirm-whether-sperm-went-inside
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1711089062how-to-confirm-whether-sperm-went-inside.webp
[blog_text] => When it comes to conceiving, couples often have questions or concerns about whether sperm has successfully fertilised an egg. This uncertainty can arise from various factors, including difficulties with natural conception or undergoing fertility treatments like IVF procedure (In Vitro Fertilisation) or IUI procedure (Intrauterine Insemination). Understanding how to confirm whether sperm went inside can help alleviate some of the anxiety and provide guidance for those on their fertility journey.
The Importance of Confirming Sperm Deposition
Confirming whether sperm has gone inside is crucial for assessing fertility potential and determining the effectiveness of assisted reproductive techniques, like IVF procedure or IUI treatment. It allows couples and fertility doctors to make informed decisions regarding future treatment plans and interventions.
Methods to Confirm Sperm Deposition
There are several methods to confirm whether sperm has successfully reached the cervix or uterus:
1) Basal Body Temperature (BBT) Tracking:
Monitoring your BBT can provide insights into your menstrual cycle and potential ovulation. This can be done using a special BBT thermometer. After ovulation, if fertilisation occurs, the BBT remains elevated due to increased progesterone levels.
2) Cervical Mucus Monitoring:
Cervical mucus changes throughout the menstrual cycle, becoming thin and stretchy around ovulation. This fertile cervical mucus helps facilitate sperm movement towards the uterus.
3) Home Ovulation Test Kits:
These kits detect luteinising hormone (LH) levels in urine, indicating an impending ovulation. Having intercourse during this fertile window increases the chances of successful sperm deposition.
4) Post-Coital Test:
Also known as the Huhner test, this examination involves collecting a sample of cervical mucus within 2-24 hours after intercourse and assessing its quality and the presence of live, motile sperm. Post-coital tests can be scheduled at a fertility clinic near you.
4) Transvaginal Ultrasound:
A transvaginal ultrasound can provide visual confirmation of sperm deposition. It allows fertility specialists to visualise the cervix, uterus and fallopian tubes to ensure proper placement during fertility procedures.
Fertility Treatments and Confirmation
1) IVF procedure:
In the IVF procedure, the fertilisation process occurs outside the body. The sperm is directly introduced to the egg in a laboratory setting. Confirmation of successful fertilisation is determined by observing embryo development after insemination.
2) IUI treatment:
During the IUI treatment, prepared sperm is inserted into the uterus using a catheter. Confirming whether sperm has fertilised an egg is essential in assessing the success of the procedure. A post-IUI ultrasound may be performed to evaluate proper catheter placement.
Confirming whether sperm has gone inside is an important aspect of the fertility journey. Various methods, including BBT tracking, cervical mucus monitoring, home ovulation test kits, post-coital tests and ultrasounds, can help determine successful sperm deposition. If you have concerns or questions about your fertility, it's recommended to consult with a fertility specialist or healthcare professional who can guide you through the process and provide personalised recommendations.
At Apollo Fertility, we are here to support you on your fertility journey. Our experienced team of doctors and state-of-the-art facilities are dedicated to providing compassionate care and personalised treatment plans. Visit our website or schedule a consultation today to take the next step towards building your family.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-22
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-22 06:31:02
[updatedDate] => 2024-03-22 06:31:02
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

How To Confirm Whether Sperm Went Inside
March 22, 2024When it comes to conceiving, couples often have questions or concerns ...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 470
[blogcat_id] => 5
[blog_title] => How To Use Ovulation Test Kits to Detect Fertility
[metaTitle] => A Guide to Detecting Fertility Using Ovulation Test Kits
[metaDescription] => Learn how ovulation test kits can help track fertility and increase chances of conceiving. Find out how to use these kits to identify your most fertile days.
[metaKeywords] =>
[seo_url] => how-to-use-ovulation-test-kits-to-detect-fertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710997114how-to-use-ovulation-test-kits-to-detect-fertility.webp
[blog_text] => If you are hoping to conceive you must have wondered about the optimal timing for intercourse. Tracking your fertility through ovulation test kits can provide valuable insights into your menstrual cycle and help you identify when you are most likely to get pregnant. In this blog, we will guide you on how to use ovulation test kits effectively, allowing you to make informed decisions on your journey towards parenthood.
What are Ovulation Test Kits?
Ovulation test kits, also known as ovulation predictor kits (OPKs), are tools that help women determine when they are ovulating. These kits detect the surge in luteinising hormone (LH) levels in a woman's urine, which occurs a day or two before ovulation.
Benefits of Ovulations Test Kits
Using an ovulation test kit can be beneficial for several reasons:
- Identifying fertile days: Knowing when you are most fertile allows you to plan intercourse accordingly, increasing your chances of conception.
- Irregular menstrual cycles: If you have irregular periods, tracking your LH surge with an ovulation test kit can help pinpoint your fertile window.
- Reduce stress: Trying to conceive can be stressful. Using an ovulation test kit takes away the guesswork and provides a clear indication of when you are most likely to conceive.
How to Use an Ovulation Test Kit
Using an ovulation test kit is simple and easy. Follow these steps for accurate results:
- Determine the length of your menstrual cycle: Start by tracking the length of your menstrual cycle. The first day of your period is considered Day 1.
- Start testing at the right time: Read the instructions provided with your kit to determine when to start testing. Generally, it is recommended to begin testing a few days before your expected ovulation date.
- Choose the right time of day: Most kits recommend testing with the first urine of the day, as it contains the highest concentration of LH. However, if instructed otherwise, follow the specific guidelines for your kit.
- Collect urine sample: Collect a urine sample in a clean container or use the test stick provided in the kit to directly collect your urine stream.
- Perform the test: Dip the test stick into the urine sample or hold it in the urine stream for the specified amount of time as mentioned in the instructions.
- Read and interpret the results: Each kit will have its own way of indicating results, so refer to the instructions for interpretation. Typically, a positive result will show two visible lines or a smiley face symbol.
Interpreting the Test Results
A positive result indicates that your LH levels have surged and ovulation is likely to occur within 24-48 hours. This is the best time to have intercourse if you are looking to conceive.
It is important to note that even if you receive a negative result, it does not necessarily mean you won't ovulate. Some women may have a short surge or miss detecting it altogether. Therefore, it is recommended to continue testing until you receive a positive result or confirm ovulation through other methods like basal body temperature (BBT) charting.
Using ovulation test kits can greatly assist in understanding your menstrual cycle and increase your chances of conceiving. However, if you have been trying to conceive for an extended period without success, it may be beneficial to consult with a fertility specialist. They can provide personalised guidance and explore additional options such as fertility treatments like IUI or IVF.
At Apollo Fertility we are here to support you every step of the way. Our experienced team of fertility specialists can provide comprehensive fertility tests and evaluations and develop personalised treatment plans tailored to your individual needs. Reach out and schedule a consultation with our experts today.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-21
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-21 04:58:34
[updatedDate] => 2024-03-21 04:58:34
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 470
[blogcat_id] => 5
[blog_title] => How To Use Ovulation Test Kits to Detect Fertility
[metaTitle] => A Guide to Detecting Fertility Using Ovulation Test Kits
[metaDescription] => Learn how ovulation test kits can help track fertility and increase chances of conceiving. Find out how to use these kits to identify your most fertile days.
[metaKeywords] =>
[seo_url] => how-to-use-ovulation-test-kits-to-detect-fertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710997114how-to-use-ovulation-test-kits-to-detect-fertility.webp
[blog_text] => If you are hoping to conceive you must have wondered about the optimal timing for intercourse. Tracking your fertility through ovulation test kits can provide valuable insights into your menstrual cycle and help you identify when you are most likely to get pregnant. In this blog, we will guide you on how to use ovulation test kits effectively, allowing you to make informed decisions on your journey towards parenthood.
What are Ovulation Test Kits?
Ovulation test kits, also known as ovulation predictor kits (OPKs), are tools that help women determine when they are ovulating. These kits detect the surge in luteinising hormone (LH) levels in a woman's urine, which occurs a day or two before ovulation.
Benefits of Ovulations Test Kits
Using an ovulation test kit can be beneficial for several reasons:
- Identifying fertile days: Knowing when you are most fertile allows you to plan intercourse accordingly, increasing your chances of conception.
- Irregular menstrual cycles: If you have irregular periods, tracking your LH surge with an ovulation test kit can help pinpoint your fertile window.
- Reduce stress: Trying to conceive can be stressful. Using an ovulation test kit takes away the guesswork and provides a clear indication of when you are most likely to conceive.
How to Use an Ovulation Test Kit
Using an ovulation test kit is simple and easy. Follow these steps for accurate results:
- Determine the length of your menstrual cycle: Start by tracking the length of your menstrual cycle. The first day of your period is considered Day 1.
- Start testing at the right time: Read the instructions provided with your kit to determine when to start testing. Generally, it is recommended to begin testing a few days before your expected ovulation date.
- Choose the right time of day: Most kits recommend testing with the first urine of the day, as it contains the highest concentration of LH. However, if instructed otherwise, follow the specific guidelines for your kit.
- Collect urine sample: Collect a urine sample in a clean container or use the test stick provided in the kit to directly collect your urine stream.
- Perform the test: Dip the test stick into the urine sample or hold it in the urine stream for the specified amount of time as mentioned in the instructions.
- Read and interpret the results: Each kit will have its own way of indicating results, so refer to the instructions for interpretation. Typically, a positive result will show two visible lines or a smiley face symbol.
Interpreting the Test Results
A positive result indicates that your LH levels have surged and ovulation is likely to occur within 24-48 hours. This is the best time to have intercourse if you are looking to conceive.
It is important to note that even if you receive a negative result, it does not necessarily mean you won't ovulate. Some women may have a short surge or miss detecting it altogether. Therefore, it is recommended to continue testing until you receive a positive result or confirm ovulation through other methods like basal body temperature (BBT) charting.
Using ovulation test kits can greatly assist in understanding your menstrual cycle and increase your chances of conceiving. However, if you have been trying to conceive for an extended period without success, it may be beneficial to consult with a fertility specialist. They can provide personalised guidance and explore additional options such as fertility treatments like IUI or IVF.
At Apollo Fertility we are here to support you every step of the way. Our experienced team of fertility specialists can provide comprehensive fertility tests and evaluations and develop personalised treatment plans tailored to your individual needs. Reach out and schedule a consultation with our experts today.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-21
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-21 04:58:34
[updatedDate] => 2024-03-21 04:58:34
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

How To Use Ovulation Test Kits to Detect Fertility
March 21, 2024If you are hoping to conceive you must have wondered about the optimal...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 469
[blogcat_id] => 19
[blog_title] => How Does Coronavirus Affect Fertility and Pregnancy?
[metaTitle] => The Impact of Coronavirus on Reproductive Health
[metaDescription] => Discover the impacts of coronavirus on fertility and pregnancy. Learn about the precautions, risks and when to seek advice from fertility specialists.
[metaKeywords] =>
[seo_url] => how-does-coronavirus-affect-fertility-and-pregnancy
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710905289how-does-coronavirus-affect-fertility-and-pregnancy.webp
[blog_text] => The COVID-19 pandemic affected every aspect of our lives, including our healthcare and reproductive plans. If you were trying to conceive or already pregnant during the pandemic, you may have had concerns about how coronavirus could impact your fertility and pregnancy journey. While the pandemic maybe behind us now, coronavirus still remains a threat and understanding its outcome on fertility and pregnancy is key. In this blog, we will explore the topic of how coronavirus affects fertility and pregnancy, provide accurate information, address common concerns, and offer guidance to those seeking fertility treatments in the face of coronavirus.
The Impact of Coronavirus and Female and Male Fertility
As of now, there is limited evidence suggesting that coronavirus directly impacts fertility in men or women. However, it's important to note that high fever and severe illness caused by the virus can temporarily affect sperm production or disrupt menstrual cycles. If you are planning to conceive naturally or through assisted reproductive technologies (ART) such as IUI treatment (intrauterine insemination) or IVF procedure (in vitro fertilisation), it is advisable to consult with a fertility specialist for personalised guidance.
Pregnancy and the Risks Associated with Coronavirus
Pregnant individuals are not at a higher risk of contracting coronavirus compared to the general population. However, pregnant individuals might be more susceptible to severe illness if they do contract the virus. It is crucial for pregnant individuals to strictly follow preventive measures such as wearing masks, practicing good hand hygiene, maintaining social distancing and seeking prenatal care regularly.
Fertility Treatments and Coronavirus
During the pandemic, many clinics implemented strict safety protocols to minimise the risk of infection, such as virtual consultations, health screenings and enhanced sanitation measures. If you believe you have been exposed to coronavirus, it is advisable to consult your fertility specialist through a virtual consultation. Your fertility specialist will provide you with guidance on next steps. They could even recommend delaying fertility treatment if you have underlying health conditions that could impact your fertility treatment.
Precautions
If you are undergoing fertility treatment such as IUI procedure or IVF procedure, it is important to follow the guidelines provided by your clinic. These may include:
- Practicing good hand hygiene and wearing masks during clinic visits
- Adhering to social distancing measures within the clinic premises
- Limiting the number of support persons accompanying you during appointments
- Conducting virtual consultations whenever possible
- Following all medications and protocols as prescribed by your fertility specialist
Testing Positive for Coronavirus While Undergoing Fertility Treatment
If you test positive for coronavirus during your fertility treatment, it is crucial to inform your fertility specialist immediately. They will guide you on whether to continue or temporarily pause the treatment based on your specific situation.
In conclusion, while the full extent of the impact of coronavirus on fertility and pregnancy is still being studied, it is evident that the virus presents unique challenges for individuals and couples planning to conceive or currently pregnant. The stress and anxiety associated with coronavirus, coupled with disruptions in treatments, highlight the importance of providing support and resources to those navigating fertility treatments and pregnancy at such times.
At Apollo Fertility, we understand the challenges faced by individuals seeking fertility treatments during such uncertain times. Our experienced team of fertility specialists follows strict safety protocols to provide you with comprehensive care while minimising the risk of exposure to coronavirus. Contact us today to schedule a consultation and take the first step on your fertility journey.
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-20 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-20 03:28:09 [updatedDate] => 2024-03-20 03:28:09 [ip_address] => 49.205.116.233 ) [_oldAttributes:yii\db\BaseActiveRecord:private] => Array ( [blog_id] => 469 [blogcat_id] => 19 [blog_title] => How Does Coronavirus Affect Fertility and Pregnancy? [metaTitle] => The Impact of Coronavirus on Reproductive Health [metaDescription] => Discover the impacts of coronavirus on fertility and pregnancy. Learn about the precautions, risks and when to seek advice from fertility specialists. [metaKeywords] => [seo_url] => how-does-coronavirus-affect-fertility-and-pregnancy [city_id] => [city_name] => [language_id] => 1 [blog_image] => blog-images/1710905289how-does-coronavirus-affect-fertility-and-pregnancy.webp [blog_text] =>The COVID-19 pandemic affected every aspect of our lives, including our healthcare and reproductive plans. If you were trying to conceive or already pregnant during the pandemic, you may have had concerns about how coronavirus could impact your fertility and pregnancy journey. While the pandemic maybe behind us now, coronavirus still remains a threat and understanding its outcome on fertility and pregnancy is key. In this blog, we will explore the topic of how coronavirus affects fertility and pregnancy, provide accurate information, address common concerns, and offer guidance to those seeking fertility treatments in the face of coronavirus.
The Impact of Coronavirus and Female and Male Fertility
As of now, there is limited evidence suggesting that coronavirus directly impacts fertility in men or women. However, it's important to note that high fever and severe illness caused by the virus can temporarily affect sperm production or disrupt menstrual cycles. If you are planning to conceive naturally or through assisted reproductive technologies (ART) such as IUI treatment (intrauterine insemination) or IVF procedure (in vitro fertilisation), it is advisable to consult with a fertility specialist for personalised guidance.
Pregnancy and the Risks Associated with Coronavirus
Pregnant individuals are not at a higher risk of contracting coronavirus compared to the general population. However, pregnant individuals might be more susceptible to severe illness if they do contract the virus. It is crucial for pregnant individuals to strictly follow preventive measures such as wearing masks, practicing good hand hygiene, maintaining social distancing and seeking prenatal care regularly.
Fertility Treatments and Coronavirus
During the pandemic, many clinics implemented strict safety protocols to minimise the risk of infection, such as virtual consultations, health screenings and enhanced sanitation measures. If you believe you have been exposed to coronavirus, it is advisable to consult your fertility specialist through a virtual consultation. Your fertility specialist will provide you with guidance on next steps. They could even recommend delaying fertility treatment if you have underlying health conditions that could impact your fertility treatment.
Precautions
If you are undergoing fertility treatment such as IUI procedure or IVF procedure, it is important to follow the guidelines provided by your clinic. These may include:
- Practicing good hand hygiene and wearing masks during clinic visits
- Adhering to social distancing measures within the clinic premises
- Limiting the number of support persons accompanying you during appointments
- Conducting virtual consultations whenever possible
- Following all medications and protocols as prescribed by your fertility specialist
Testing Positive for Coronavirus While Undergoing Fertility Treatment
If you test positive for coronavirus during your fertility treatment, it is crucial to inform your fertility specialist immediately. They will guide you on whether to continue or temporarily pause the treatment based on your specific situation.
In conclusion, while the full extent of the impact of coronavirus on fertility and pregnancy is still being studied, it is evident that the virus presents unique challenges for individuals and couples planning to conceive or currently pregnant. The stress and anxiety associated with coronavirus, coupled with disruptions in treatments, highlight the importance of providing support and resources to those navigating fertility treatments and pregnancy at such times.
At Apollo Fertility, we understand the challenges faced by individuals seeking fertility treatments during such uncertain times. Our experienced team of fertility specialists follows strict safety protocols to provide you with comprehensive care while minimising the risk of exposure to coronavirus. Contact us today to schedule a consultation and take the first step on your fertility journey.
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-20 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-20 03:28:09 [updatedDate] => 2024-03-20 03:28:09 [ip_address] => 49.205.116.233 ) [_related:yii\db\BaseActiveRecord:private] => Array ( ) [_relationsDependencies:yii\db\BaseActiveRecord:private] => Array ( ) [_errors:yii\base\Model:private] => [_validators:yii\base\Model:private] => [_scenario:yii\base\Model:private] => default [_events:yii\base\Component:private] => Array ( ) [_eventWildcards:yii\base\Component:private] => Array ( ) [_behaviors:yii\base\Component:private] => Array ( ) )
How Does Coronavirus Affect Fertility and Pregnancy?
March 20, 2024The COVID-19 pandemic affected every aspect of our lives, including ou...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 468
[blogcat_id] => 5
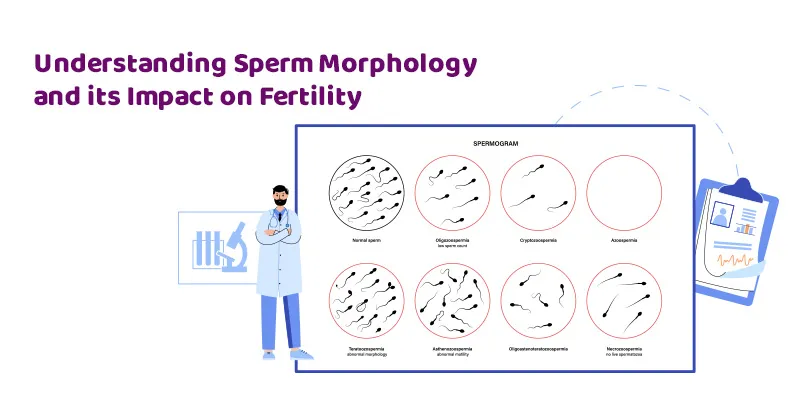
[blog_title] => Sperm Morphology – What Is It & How Does It Affect Fertility
[metaTitle] => Understanding Sperm Morphology and its Impact on Fertility
[metaDescription] => Discover how sperm morphology impacts fertility. Learn about abnormal sperm morphology causes and treatments. Enhance your understanding of male infertility now.
[metaKeywords] =>
[seo_url] => sperm-morphology-what-is-it-how-does-it-affect-fertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710818578sperm-morphology-what-is-it-how-does-it-affect-fertility.webp
[blog_text] => The topic of fertility is important for both men and women as good reproductive health is crucial in both partners to conceive. Consequently, it is worth noting that male infertility accounts for about 30-40% of all cases of infertility. One important aspect of male fertility is sperm morphology. In this blog, we will explain what is sperm morphology and how it affects fertility.
What is Sperm Morphology?
Sperm morphology refers to the size and shape of sperm. In order for sperm to be considered normal, they should have a healthy shape and structure. Abnormalities in sperm morphology can make it more difficult for them to reach and fertilise an egg.
Understanding How Sperm Morphology Affects Fertility
Sperm with abnormal morphology may have difficulty swimming properly or penetrating the egg. This can significantly reduce the chances of successful fertilisation and pregnancy. Even if fertilisation occurs, abnormal sperm morphology can increase the risk of miscarriage or genetic abnormalities in the embryo.
Causes of Abnormal Sperm Morphology
There are several factors that can contribute to abnormal sperm morphology:
- Genetic Factors: Some men may have a genetic predisposition to abnormal sperm morphology.
- Lifestyle Choices: Certain lifestyle choices such as smoking, excessive alcohol consumption, drug use, poor diet and lack of exercise can negatively impact sperm morphology.
- Hormonal Imbalances: Hormonal imbalances, such as low testosterone levels, can affect sperm production and lead to abnormalities.
- Environmental Factors: Exposure to environmental toxins like pesticides, chemicals, radiation or high temperatures (such as from tight clothing or hot tubs) can affect sperm quality.
- Medical Conditions: Certain medical conditions like varicocele (enlarged veins in the scrotum), infections or hormonal disorders can also contribute to abnormal sperm morphology.
Treatment for Abnormal Sperm Morphology
There are several treatment options available for men with abnormal sperm morphology. The most common approach is to undergo fertility treatments such as Intrauterine Insemination (IUI) or In Vitro Fertilisation (IVF).
In IUI treatment, sperm with abnormal morphology can be separated from healthy sperm and directly inserted into the woman's uterus during her fertile period. This increases the chances of successful fertilisation.
In IVF procedure, the woman's eggs are retrieved and fertilised with the partner's or a donor's sperm in a laboratory. The resulting embryos are then transferred to the woman's uterus. By bypassing natural fertilisation, An IVF procedure can overcome issues related to abnormal sperm morphology.
Since this is not a one size fits all situation, a fertility specialist will conduct fertility tests and thorough physical evaluations and recommend a treatment that best suits the individuals need. The customised treatment plan by the fertility specialist will depend on various factors, including the underlying cause of the abnormal morphology and the couple's overall health.
In conclusion, recognising the importance of fertility for both men and women is paramount, with male infertility comprising a significant portion of infertility cases. Exploring sperm morphology provides insights into its pivotal role in conception. By consulting fertility specialists and devising personalised treatment plans, addressing underlying causes becomes key to enhancing fertility prospects. Ultimately, understanding and addressing male fertility issues contribute to a holistic approach in the journey toward parenthood.
If you have concerns about your fertility or are experiencing difficulty conceiving, seek the expert guidance of a fertility specialist at Apollo Fertility. The highly experienced team of fertility doctors offers comprehensive fertility treatments tailored to individual needs. With our compassionate and expert team, we are here to support you on your journey to parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-19
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-19 03:22:58
[updatedDate] => 2024-03-19 03:22:58
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 468
[blogcat_id] => 5
[blog_title] => Sperm Morphology – What Is It & How Does It Affect Fertility
[metaTitle] => Understanding Sperm Morphology and its Impact on Fertility
[metaDescription] => Discover how sperm morphology impacts fertility. Learn about abnormal sperm morphology causes and treatments. Enhance your understanding of male infertility now.
[metaKeywords] =>
[seo_url] => sperm-morphology-what-is-it-how-does-it-affect-fertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710818578sperm-morphology-what-is-it-how-does-it-affect-fertility.webp
[blog_text] => The topic of fertility is important for both men and women as good reproductive health is crucial in both partners to conceive. Consequently, it is worth noting that male infertility accounts for about 30-40% of all cases of infertility. One important aspect of male fertility is sperm morphology. In this blog, we will explain what is sperm morphology and how it affects fertility.
What is Sperm Morphology?
Sperm morphology refers to the size and shape of sperm. In order for sperm to be considered normal, they should have a healthy shape and structure. Abnormalities in sperm morphology can make it more difficult for them to reach and fertilise an egg.
Understanding How Sperm Morphology Affects Fertility
Sperm with abnormal morphology may have difficulty swimming properly or penetrating the egg. This can significantly reduce the chances of successful fertilisation and pregnancy. Even if fertilisation occurs, abnormal sperm morphology can increase the risk of miscarriage or genetic abnormalities in the embryo.
Causes of Abnormal Sperm Morphology
There are several factors that can contribute to abnormal sperm morphology:
- Genetic Factors: Some men may have a genetic predisposition to abnormal sperm morphology.
- Lifestyle Choices: Certain lifestyle choices such as smoking, excessive alcohol consumption, drug use, poor diet and lack of exercise can negatively impact sperm morphology.
- Hormonal Imbalances: Hormonal imbalances, such as low testosterone levels, can affect sperm production and lead to abnormalities.
- Environmental Factors: Exposure to environmental toxins like pesticides, chemicals, radiation or high temperatures (such as from tight clothing or hot tubs) can affect sperm quality.
- Medical Conditions: Certain medical conditions like varicocele (enlarged veins in the scrotum), infections or hormonal disorders can also contribute to abnormal sperm morphology.
Treatment for Abnormal Sperm Morphology
There are several treatment options available for men with abnormal sperm morphology. The most common approach is to undergo fertility treatments such as Intrauterine Insemination (IUI) or In Vitro Fertilisation (IVF).
In IUI treatment, sperm with abnormal morphology can be separated from healthy sperm and directly inserted into the woman's uterus during her fertile period. This increases the chances of successful fertilisation.
In IVF procedure, the woman's eggs are retrieved and fertilised with the partner's or a donor's sperm in a laboratory. The resulting embryos are then transferred to the woman's uterus. By bypassing natural fertilisation, An IVF procedure can overcome issues related to abnormal sperm morphology.
Since this is not a one size fits all situation, a fertility specialist will conduct fertility tests and thorough physical evaluations and recommend a treatment that best suits the individuals need. The customised treatment plan by the fertility specialist will depend on various factors, including the underlying cause of the abnormal morphology and the couple's overall health.
In conclusion, recognising the importance of fertility for both men and women is paramount, with male infertility comprising a significant portion of infertility cases. Exploring sperm morphology provides insights into its pivotal role in conception. By consulting fertility specialists and devising personalised treatment plans, addressing underlying causes becomes key to enhancing fertility prospects. Ultimately, understanding and addressing male fertility issues contribute to a holistic approach in the journey toward parenthood.
If you have concerns about your fertility or are experiencing difficulty conceiving, seek the expert guidance of a fertility specialist at Apollo Fertility. The highly experienced team of fertility doctors offers comprehensive fertility treatments tailored to individual needs. With our compassionate and expert team, we are here to support you on your journey to parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-19
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-19 03:22:58
[updatedDate] => 2024-03-19 03:22:58
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)
Sperm Morphology – What Is It & How Does It Affect Fertility
March 19, 2024The topic of fertility is important for both men and women as good rep...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 467
[blogcat_id] => 12
[blog_title] => How Can ICSI Help in Infertility
[metaTitle] => Understanding How ICSI Can Help Treat Infertility
[metaDescription] => Discover how ICSI can assist in overcoming infertility. Learn about the process, success rates, and why it may be a suitable option for you.
[metaKeywords] =>
[seo_url] => how-can-icsi-help-in-infertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710723054how-can-icsi-help-in-infertility.webp
[blog_text] => Female and male infertility is a complex issue that affects many couples on their journey to conceive. It can be overwhelming and emotionally draining, but it is important to remember that you are not alone. There are various fertility treatments available to help individuals and couples overcome infertility and realise their dreams of starting a family. One such treatment is Intracytoplasmic Sperm Injection (ICSI), which has revolutionised the field of assisted reproduction. In this blog, we will explore what ICSI is, how it works, its success rates, and why it may be a suitable option for you.
What is ICSI?
ICSI is an advanced form of in vitro fertilisation (IVF). It involves the direct injection of a single sperm into the cytoplasm of an egg to facilitate fertilisation. This technique is particularly beneficial for couples experiencing male infertility issues such as low sperm count, poor sperm motility or abnormal sperm morphology.
Understanding How ICSI Works
The ICSI procedure begins with the collection of eggs from the female partner through ovarian stimulation. Once the eggs are retrieved, they are carefully examined under a microscope. Subsequently, a highly skilled embryologist selects a healthy-looking sperm and immobilises it using microscopic tools. The selected sperm is then injected directly into the egg using a delicate needle.
After fertilisation occurs, the embryo undergoes development in a controlled laboratory environment before being transferred back into the woman's uterus during her IVF procedure. The success rates of ICSI largely depend on various factors such as the quality of eggs and sperm used, maternal age and the expertise of the fertility clinic.
Success Rates of ICSI
ICSI has been a game-changer for couples struggling with male infertility issues. The success rates of ICSI vary depending on individual circumstances but have shown promising results overall. According to studies, the success rates for ICSI range from 40% to 70% per cycle. These rates may differ depending on factors such as maternal age, underlying infertility causes and the experience of the fertility clinic.
Why Choose ICSI?
ICSI offers hope to couples facing male infertility issues by providing an effective solution. Here are some reasons why you might consider choosing ICSI:
- Male infertility factor: If your partner is diagnosed with male infertility issues such as low sperm count or poor sperm motility, ICSI can help overcome these challenges and increase the chances of successful fertilisation.
- Previous IVF failures: If you have undergone multiple unsuccessful IVF procedures in the past, incorporating ICSI may improve your chances of a successful pregnancy by addressing potential fertilisation issues.
- Fertility preservation: In cases where there is a need for fertility preservation due to medical reasons, such as cancer treatment, ICSI can be utilised to freeze embryos for future use.
- Genetic testing: ICSI can be combined with preimplantation genetic testing (PGT) to screen embryos for certain genetic disorders before transfer, reducing the risk of passing on inherited conditions to your child.
- Unexplained infertility: In cases where the cause of infertility is unknown or unexplained, ICSI can help bypass any unidentified barriers to fertilisation and increase your chances of conceiving.
If you are considering ICSI or have further questions about fertility treatments or options available to you, it is important to consult with a qualified fertility specialist. They will be able to assess your individual situation, provide personalised guidance, and help you make informed decisions regarding your fertility journey.
At Apollo Fertility, our team of expert fertility specialists are here to support and guide you through every step of the way. Schedule a consultation today and take the first step towards achieving your dreams of parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-18
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-18 00:50:54
[updatedDate] => 2024-03-18 00:50:54
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 467
[blogcat_id] => 12
[blog_title] => How Can ICSI Help in Infertility
[metaTitle] => Understanding How ICSI Can Help Treat Infertility
[metaDescription] => Discover how ICSI can assist in overcoming infertility. Learn about the process, success rates, and why it may be a suitable option for you.
[metaKeywords] =>
[seo_url] => how-can-icsi-help-in-infertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710723054how-can-icsi-help-in-infertility.webp
[blog_text] => Female and male infertility is a complex issue that affects many couples on their journey to conceive. It can be overwhelming and emotionally draining, but it is important to remember that you are not alone. There are various fertility treatments available to help individuals and couples overcome infertility and realise their dreams of starting a family. One such treatment is Intracytoplasmic Sperm Injection (ICSI), which has revolutionised the field of assisted reproduction. In this blog, we will explore what ICSI is, how it works, its success rates, and why it may be a suitable option for you.
What is ICSI?
ICSI is an advanced form of in vitro fertilisation (IVF). It involves the direct injection of a single sperm into the cytoplasm of an egg to facilitate fertilisation. This technique is particularly beneficial for couples experiencing male infertility issues such as low sperm count, poor sperm motility or abnormal sperm morphology.
Understanding How ICSI Works
The ICSI procedure begins with the collection of eggs from the female partner through ovarian stimulation. Once the eggs are retrieved, they are carefully examined under a microscope. Subsequently, a highly skilled embryologist selects a healthy-looking sperm and immobilises it using microscopic tools. The selected sperm is then injected directly into the egg using a delicate needle.
After fertilisation occurs, the embryo undergoes development in a controlled laboratory environment before being transferred back into the woman's uterus during her IVF procedure. The success rates of ICSI largely depend on various factors such as the quality of eggs and sperm used, maternal age and the expertise of the fertility clinic.
Success Rates of ICSI
ICSI has been a game-changer for couples struggling with male infertility issues. The success rates of ICSI vary depending on individual circumstances but have shown promising results overall. According to studies, the success rates for ICSI range from 40% to 70% per cycle. These rates may differ depending on factors such as maternal age, underlying infertility causes and the experience of the fertility clinic.
Why Choose ICSI?
ICSI offers hope to couples facing male infertility issues by providing an effective solution. Here are some reasons why you might consider choosing ICSI:
- Male infertility factor: If your partner is diagnosed with male infertility issues such as low sperm count or poor sperm motility, ICSI can help overcome these challenges and increase the chances of successful fertilisation.
- Previous IVF failures: If you have undergone multiple unsuccessful IVF procedures in the past, incorporating ICSI may improve your chances of a successful pregnancy by addressing potential fertilisation issues.
- Fertility preservation: In cases where there is a need for fertility preservation due to medical reasons, such as cancer treatment, ICSI can be utilised to freeze embryos for future use.
- Genetic testing: ICSI can be combined with preimplantation genetic testing (PGT) to screen embryos for certain genetic disorders before transfer, reducing the risk of passing on inherited conditions to your child.
- Unexplained infertility: In cases where the cause of infertility is unknown or unexplained, ICSI can help bypass any unidentified barriers to fertilisation and increase your chances of conceiving.
If you are considering ICSI or have further questions about fertility treatments or options available to you, it is important to consult with a qualified fertility specialist. They will be able to assess your individual situation, provide personalised guidance, and help you make informed decisions regarding your fertility journey.
At Apollo Fertility, our team of expert fertility specialists are here to support and guide you through every step of the way. Schedule a consultation today and take the first step towards achieving your dreams of parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-18
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-18 00:50:54
[updatedDate] => 2024-03-18 00:50:54
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

How Can ICSI Help in Infertility
March 18, 2024Female and male infertility is a complex issue that affects many coupl...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 466
[blogcat_id] => 8
[blog_title] => Treatments For Men with Low Sperm Count
[metaTitle] => Treatments for Men with Low Sperm Count: Options and Hope
[metaDescription] => Learn about the treatments for men with low sperm count and discover how taking proactive steps towards improving fertility can increase chances of conception.
[metaKeywords] =>
[seo_url] => treatments-for-men-with-low-sperm-count
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710465055treatments-for-men-with-low-sperm-count.webp
[blog_text] => If you and your partner have been struggling to conceive, it is important to remember that infertility is not solely a female issue. In fact, male infertility accounts for nearly 40% of all infertility cases. If you've been diagnosed with a low sperm count, also known as oligospermia, there are treatments available that can increase your chances of achieving a successful pregnancy. In this article, we will explore the different treatment options for men with low sperm count and provide you with hope for starting or expanding your family.
Lifestyle Changes
Before exploring medical interventions, it is essential to focus on making positive lifestyle changes that can potentially improve your sperm count. Start by adopting a healthier diet rich in antioxidants, vitamins, and minerals. Foods such as fruits, vegetables, whole grains, nuts, and lean proteins support overall reproductive health. Regular exercise and maintaining a healthy weight also contribute to optimal sperm production. Additionally, avoid smoking, excessive alcohol consumption, recreational drug use and exposure to environmental toxins like pesticides or industrial chemicals as they are factors causing male infertility issues.
Medications
In some cases, medication may be prescribed by your fertility specialist to address an underlying condition or improve sperm production. Your fertility specialist may recommend Clomiphene citrate or gonadotropin injections, which stimulate the production of hormones that regulate sperm production. These medications can increase both the quantity and quality of sperm.
Assisted Reproductive Technologies (ART)
If lifestyle changes and medication alone do not yield significant results, ART may be recommended:
- Intrauterine Insemination (IUI): IUI treatment involves the placement of washed and concentrated sperm directly into the uterus during ovulation. This procedure can bypass barriers in the reproductive system and increase the chances of fertilisation.
- In Vitro Fertilisation (IVF): IVF procedure is a highly effective ART technique that involves fertilising an egg with sperm in a laboratory setting. The resulting embryos are then transferred to the woman's uterus. IVF procedure can be combined with additional procedures, such as Intracytoplasmic Sperm Injection (ICSI), where a single sperm is injected directly into an egg, to overcome severe male infertility issues.
Surgical Interventions
In some cases, your fertility specialist might recommend surgical interventions to address anatomical abnormalities that affect sperm production or delivery. Procedures such as varicocelectomy (repairing enlarged veins in the scrotum) or vasectomy reversal can improve sperm count and mobility. However, it is important to note that not all cases of low sperm count can be resolved through surgery.
In conclusion, a diagnosis of low sperm count doesn't mean the end of your journey towards parenthood. With a range of treatment options available, including lifestyle changes, medications and assisted reproductive technologies, there is hope for improving your fertility and increasing your chances of conception. Remember to consult with a fertility specialist who can guide you through the process and tailor a treatment plan specific to your needs.
To explore your options further or to schedule a consultation, reach out to Apollo Fertility, a renowned chain of clinics that offers comprehensive fertility treatments with a balanced approach towards both female and male infertility.
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-15 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-15 01:08:49 [updatedDate] => 2024-03-15 01:10:55 [ip_address] => 49.205.116.233 ) [_oldAttributes:yii\db\BaseActiveRecord:private] => Array ( [blog_id] => 466 [blogcat_id] => 8 [blog_title] => Treatments For Men with Low Sperm Count [metaTitle] => Treatments for Men with Low Sperm Count: Options and Hope [metaDescription] => Learn about the treatments for men with low sperm count and discover how taking proactive steps towards improving fertility can increase chances of conception. [metaKeywords] => [seo_url] => treatments-for-men-with-low-sperm-count [city_id] => [city_name] => [language_id] => 1 [blog_image] => blog-images/1710465055treatments-for-men-with-low-sperm-count.webp [blog_text] =>If you and your partner have been struggling to conceive, it is important to remember that infertility is not solely a female issue. In fact, male infertility accounts for nearly 40% of all infertility cases. If you've been diagnosed with a low sperm count, also known as oligospermia, there are treatments available that can increase your chances of achieving a successful pregnancy. In this article, we will explore the different treatment options for men with low sperm count and provide you with hope for starting or expanding your family.
Lifestyle Changes
Before exploring medical interventions, it is essential to focus on making positive lifestyle changes that can potentially improve your sperm count. Start by adopting a healthier diet rich in antioxidants, vitamins, and minerals. Foods such as fruits, vegetables, whole grains, nuts, and lean proteins support overall reproductive health. Regular exercise and maintaining a healthy weight also contribute to optimal sperm production. Additionally, avoid smoking, excessive alcohol consumption, recreational drug use and exposure to environmental toxins like pesticides or industrial chemicals as they are factors causing male infertility issues.
Medications
In some cases, medication may be prescribed by your fertility specialist to address an underlying condition or improve sperm production. Your fertility specialist may recommend Clomiphene citrate or gonadotropin injections, which stimulate the production of hormones that regulate sperm production. These medications can increase both the quantity and quality of sperm.
Assisted Reproductive Technologies (ART)
If lifestyle changes and medication alone do not yield significant results, ART may be recommended:
- Intrauterine Insemination (IUI): IUI treatment involves the placement of washed and concentrated sperm directly into the uterus during ovulation. This procedure can bypass barriers in the reproductive system and increase the chances of fertilisation.
- In Vitro Fertilisation (IVF): IVF procedure is a highly effective ART technique that involves fertilising an egg with sperm in a laboratory setting. The resulting embryos are then transferred to the woman's uterus. IVF procedure can be combined with additional procedures, such as Intracytoplasmic Sperm Injection (ICSI), where a single sperm is injected directly into an egg, to overcome severe male infertility issues.
Surgical Interventions
In some cases, your fertility specialist might recommend surgical interventions to address anatomical abnormalities that affect sperm production or delivery. Procedures such as varicocelectomy (repairing enlarged veins in the scrotum) or vasectomy reversal can improve sperm count and mobility. However, it is important to note that not all cases of low sperm count can be resolved through surgery.
In conclusion, a diagnosis of low sperm count doesn't mean the end of your journey towards parenthood. With a range of treatment options available, including lifestyle changes, medications and assisted reproductive technologies, there is hope for improving your fertility and increasing your chances of conception. Remember to consult with a fertility specialist who can guide you through the process and tailor a treatment plan specific to your needs.
To explore your options further or to schedule a consultation, reach out to Apollo Fertility, a renowned chain of clinics that offers comprehensive fertility treatments with a balanced approach towards both female and male infertility.
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-15 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-15 01:08:49 [updatedDate] => 2024-03-15 01:10:55 [ip_address] => 49.205.116.233 ) [_related:yii\db\BaseActiveRecord:private] => Array ( ) [_relationsDependencies:yii\db\BaseActiveRecord:private] => Array ( ) [_errors:yii\base\Model:private] => [_validators:yii\base\Model:private] => [_scenario:yii\base\Model:private] => default [_events:yii\base\Component:private] => Array ( ) [_eventWildcards:yii\base\Component:private] => Array ( ) [_behaviors:yii\base\Component:private] => Array ( ) )
Treatments For Men with Low Sperm Count
March 15, 2024If you and your partner have been struggling to conceive, it is import...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 465
[blogcat_id] => 8
[blog_title] => Low Sperm Count – Causes & Treatment
[metaTitle] => Low Sperm Count: Understanding Male Infertility
[metaDescription] => Discover what low sperm count means and the causes, treatment options and lifestyle changes to improve sperm count.
[metaKeywords] =>
[seo_url] => low-sperm-count-causes-treatment
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710394782low-sperm-count-causes-treatment.webp
[blog_text] => In current times, many couples are facing challenges when it comes to conceiving. While female infertility issues are widely known about. It is important to consider male infertility as well. One common issue faced by men is low sperm count, which can significantly impact fertility. In this blog, we will explore the causes of low sperm count and discuss treatment options that can help increase your chances of conception.
What is low sperm count?
Low sperm count, also known as oligospermia, refers to having fewer than 15 million sperm per millilitre of semen. It is one of the leading causes of male infertility and can make it difficult for couples to conceive naturally.
Causes of low sperm count
Several factors can contribute to low sperm count:
- Medical conditions: Certain medical conditions such as varicocele (enlarged veins in the testicles), infections, hormonal imbalances or genetic disorders can affect sperm production.
- Lifestyle choices: Unhealthy lifestyle habits such as smoking, excessive alcohol consumption, drug use, obesity and exposure to toxins or radiation can lower sperm count.
- Age: Just like women experience a decline in fertility with age, men also undergo changes that can affect their sperm quality and quantity as they get older.
- Stress: Chronic stress can interfere with hormone production and negatively impact overall reproductive health.
- Medications: Some medications like certain antibiotics or testosterone replacement therapy may temporarily reduce sperm production.
How is low sperm count diagnosed?
If you suspect you have a low sperm count, it is important to consult a fertility specialist who will conduct fertility tests and thorough health evaluations. The diagnostic process may involve:
- Physical examination: The fertility doctor will examine your genitals for any abnormalities or signs of infection.
- Semen analysis: This test measures the quantity, quality and movement (motility) of your sperm. It is the primary tool used to diagnose low sperm count.
- Hormone testing: Blood tests can determine hormonal imbalances that may be affecting sperm production.
- Genetic testing: In some cases, genetic testing may be recommended to identify any chromosomal abnormalities that could contribute to low sperm count.
Treatment for low sperm count
The treatment options for low sperm count depend on the underlying cause and severity of the condition. Here are some common approaches:
- Lifestyle changes: Making positive changes to your lifestyle can significantly improve sperm count. Quitting smoking, reducing alcohol consumption, managing stress, maintaining a healthy weight through regular exercise and a balanced diet and avoiding exposure to toxins can all positively impact fertility.
- Medications: Depending on the cause of low sperm count, your doctor may prescribe medications to address hormonal imbalances or treat infections that could be affecting sperm production.
- Assisted reproductive techniques: In cases where natural conception is not possible, assisted reproductive techniques such as IUI procedure (intrauterine insemination) or IVF procedure (in vitro fertilisation) may be recommended. These procedures involve collecting sperm and introducing them into the female partner's reproductive system or fertilising eggs outside the body before transferring them into the uterus.
- Surgical interventions: If an anatomical issue like varicocele is causing low sperm count, your fertility specialist may recommend surgery to correct the problem.
In conclusion, understanding the complexities of male infertility, particularly low sperm count, is crucial for couples striving to conceive. By recognising the various factors contributing to low sperm count and seeking guidance from fertility specialists, couples can navigate this journey more effectively. From lifestyle adjustments to medical interventions and assisted reproductive techniques, there are viable pathways toward addressing male infertility and increasing the likelihood of conception. With proactive measures and expert support, couples can embark on their parenthood journey with renewed hope and optimism.
At Apollo Fertility we are here to support you every step of the way. Our team of experienced fertility specialists offers personalised treatment plans tailored to your specific needs. Schedule a consultation today and let us guide you on your path towards parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-14
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-14 05:39:42
[updatedDate] => 2024-03-14 05:39:42
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 465
[blogcat_id] => 8
[blog_title] => Low Sperm Count – Causes & Treatment
[metaTitle] => Low Sperm Count: Understanding Male Infertility
[metaDescription] => Discover what low sperm count means and the causes, treatment options and lifestyle changes to improve sperm count.
[metaKeywords] =>
[seo_url] => low-sperm-count-causes-treatment
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710394782low-sperm-count-causes-treatment.webp
[blog_text] => In current times, many couples are facing challenges when it comes to conceiving. While female infertility issues are widely known about. It is important to consider male infertility as well. One common issue faced by men is low sperm count, which can significantly impact fertility. In this blog, we will explore the causes of low sperm count and discuss treatment options that can help increase your chances of conception.
What is low sperm count?
Low sperm count, also known as oligospermia, refers to having fewer than 15 million sperm per millilitre of semen. It is one of the leading causes of male infertility and can make it difficult for couples to conceive naturally.
Causes of low sperm count
Several factors can contribute to low sperm count:
- Medical conditions: Certain medical conditions such as varicocele (enlarged veins in the testicles), infections, hormonal imbalances or genetic disorders can affect sperm production.
- Lifestyle choices: Unhealthy lifestyle habits such as smoking, excessive alcohol consumption, drug use, obesity and exposure to toxins or radiation can lower sperm count.
- Age: Just like women experience a decline in fertility with age, men also undergo changes that can affect their sperm quality and quantity as they get older.
- Stress: Chronic stress can interfere with hormone production and negatively impact overall reproductive health.
- Medications: Some medications like certain antibiotics or testosterone replacement therapy may temporarily reduce sperm production.
How is low sperm count diagnosed?
If you suspect you have a low sperm count, it is important to consult a fertility specialist who will conduct fertility tests and thorough health evaluations. The diagnostic process may involve:
- Physical examination: The fertility doctor will examine your genitals for any abnormalities or signs of infection.
- Semen analysis: This test measures the quantity, quality and movement (motility) of your sperm. It is the primary tool used to diagnose low sperm count.
- Hormone testing: Blood tests can determine hormonal imbalances that may be affecting sperm production.
- Genetic testing: In some cases, genetic testing may be recommended to identify any chromosomal abnormalities that could contribute to low sperm count.
Treatment for low sperm count
The treatment options for low sperm count depend on the underlying cause and severity of the condition. Here are some common approaches:
- Lifestyle changes: Making positive changes to your lifestyle can significantly improve sperm count. Quitting smoking, reducing alcohol consumption, managing stress, maintaining a healthy weight through regular exercise and a balanced diet and avoiding exposure to toxins can all positively impact fertility.
- Medications: Depending on the cause of low sperm count, your doctor may prescribe medications to address hormonal imbalances or treat infections that could be affecting sperm production.
- Assisted reproductive techniques: In cases where natural conception is not possible, assisted reproductive techniques such as IUI procedure (intrauterine insemination) or IVF procedure (in vitro fertilisation) may be recommended. These procedures involve collecting sperm and introducing them into the female partner's reproductive system or fertilising eggs outside the body before transferring them into the uterus.
- Surgical interventions: If an anatomical issue like varicocele is causing low sperm count, your fertility specialist may recommend surgery to correct the problem.
In conclusion, understanding the complexities of male infertility, particularly low sperm count, is crucial for couples striving to conceive. By recognising the various factors contributing to low sperm count and seeking guidance from fertility specialists, couples can navigate this journey more effectively. From lifestyle adjustments to medical interventions and assisted reproductive techniques, there are viable pathways toward addressing male infertility and increasing the likelihood of conception. With proactive measures and expert support, couples can embark on their parenthood journey with renewed hope and optimism.
At Apollo Fertility we are here to support you every step of the way. Our team of experienced fertility specialists offers personalised treatment plans tailored to your specific needs. Schedule a consultation today and let us guide you on your path towards parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-14
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-14 05:39:42
[updatedDate] => 2024-03-14 05:39:42
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)
Low Sperm Count – Causes & Treatment
March 14, 2024In current times, many couples are facing challenges when it comes to ...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 464
[blogcat_id] => 8
[blog_title] => Do Men Have Biological Clocks — What Is a Biological Clock?
[metaTitle] => Understanding Male Fertility and the Concept of Biological Clocks
[metaDescription] => Learn if men have biological clocks and about the factors impacting male fertility. Gain insights into how the male biological clock affects chances of conception.
[metaKeywords] =>
[seo_url] => do-men-have-biological-clocks-what-is-a-biological-clock
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710292477#418083.png
[blog_text] => When it comes to the topic of fertility, discussions often revolve around women and their biological clocks. However, it is important to recognise that men also have biological clocks that can impact fertility. In this blog, we will explore the concept of male fertility, as well as male infertility, and shed light on whether men have biological clocks.
What is a Biological Clock?
The term "biological clock" refers to the natural decline in reproductive potential as individuals age. In women, this decline is well-known and is primarily associated with a decrease in egg quality and quantity. However, research suggests that men also experience a decline in fertility as they grow older.
The Impact of Age on Male Infertility
Unlike women who experience a clear-cut decline in fertility with age, men tend to have a more gradual decrease in reproductive potential. Nevertheless, studies have shown that advancing age can lead to various challenges for men trying to conceive:
- Decreased Sperm Quality: As men age, the quality of their sperm may decline. This can affect sperm count, motility (ability to swim) and morphology (shape). These changes can reduce the chances of successful fertilisation.
- Increased Risk of Genetic Abnormalities: Advanced paternal age has been linked to an increased risk of genetic abnormalities in offspring. For instance, children born to older fathers may have higher rates of certain conditions like autism or schizophrenia.
- Reduced Sexual Function: Aging can also impact sexual function, including erectile dysfunction or a decrease in libido. These factors can hinder conception and lead to additional stress and emotional strain.
Promoting Male Fertility
While men may face challenges as they age, there are steps they can take to support their fertility:
- Lead a Healthy Lifestyle: Maintaining a healthy weight, exercising regularly, getting enough sleep, consuming fertility foods and managing stress can positively impact male fertility. Additionally, avoiding tobacco, excessive alcohol consumption and illicit drug use is crucial for reproductive health, as these habits increase the risk of male infertility.
- Regular Fertility Tests: Undergoing regular fertility tests can help identify any potential issues early on. These tests evaluate sperm count, motility, morphology as well as genetic factors that may affect fertility.
- Seek Medical Advice: Consulting with a fertility specialist is essential for couples struggling to conceive. A fertility specialist can assess both partners' fertility and provide personalised recommendations or treatment options tailored to their specific needs.
- Consider Fertility Preservation: For men who want to delay parenthood or anticipate potential future fertility issues, fertility preservation options such as sperm freezing can offer peace of mind.
In conclusion, the biological clock exists for men and can cause male infertility through factors such as decreased sperm quality, increased risk of genetic abnormalities and reduced sexual function with age. Adopting a healthy lifestyle, undergoing regular fertility tests, seeking medical advice and considering fertility preservation are vital steps for addressing concerns related to male infertility. Understanding and addressing male infertility is crucial for couples striving to conceive and build families.
At Apollo Fertility, we understand the challenges and concerns surrounding fertility. Our renowned clinics offer comprehensive evaluations and personalised treatment options for both men and women. Whether you're considering IVF procedure, IUI treatment, or fertility preservation, our expert team of fertility specialists is here to support and guide you. Schedule a visit with us today and embark on your journey towards parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-13
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-13 01:12:46
[updatedDate] => 2024-03-13 01:14:37
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 464
[blogcat_id] => 8
[blog_title] => Do Men Have Biological Clocks — What Is a Biological Clock?
[metaTitle] => Understanding Male Fertility and the Concept of Biological Clocks
[metaDescription] => Learn if men have biological clocks and about the factors impacting male fertility. Gain insights into how the male biological clock affects chances of conception.
[metaKeywords] =>
[seo_url] => do-men-have-biological-clocks-what-is-a-biological-clock
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710292477#418083.png
[blog_text] => When it comes to the topic of fertility, discussions often revolve around women and their biological clocks. However, it is important to recognise that men also have biological clocks that can impact fertility. In this blog, we will explore the concept of male fertility, as well as male infertility, and shed light on whether men have biological clocks.
What is a Biological Clock?
The term "biological clock" refers to the natural decline in reproductive potential as individuals age. In women, this decline is well-known and is primarily associated with a decrease in egg quality and quantity. However, research suggests that men also experience a decline in fertility as they grow older.
The Impact of Age on Male Infertility
Unlike women who experience a clear-cut decline in fertility with age, men tend to have a more gradual decrease in reproductive potential. Nevertheless, studies have shown that advancing age can lead to various challenges for men trying to conceive:
- Decreased Sperm Quality: As men age, the quality of their sperm may decline. This can affect sperm count, motility (ability to swim) and morphology (shape). These changes can reduce the chances of successful fertilisation.
- Increased Risk of Genetic Abnormalities: Advanced paternal age has been linked to an increased risk of genetic abnormalities in offspring. For instance, children born to older fathers may have higher rates of certain conditions like autism or schizophrenia.
- Reduced Sexual Function: Aging can also impact sexual function, including erectile dysfunction or a decrease in libido. These factors can hinder conception and lead to additional stress and emotional strain.
Promoting Male Fertility
While men may face challenges as they age, there are steps they can take to support their fertility:
- Lead a Healthy Lifestyle: Maintaining a healthy weight, exercising regularly, getting enough sleep, consuming fertility foods and managing stress can positively impact male fertility. Additionally, avoiding tobacco, excessive alcohol consumption and illicit drug use is crucial for reproductive health, as these habits increase the risk of male infertility.
- Regular Fertility Tests: Undergoing regular fertility tests can help identify any potential issues early on. These tests evaluate sperm count, motility, morphology as well as genetic factors that may affect fertility.
- Seek Medical Advice: Consulting with a fertility specialist is essential for couples struggling to conceive. A fertility specialist can assess both partners' fertility and provide personalised recommendations or treatment options tailored to their specific needs.
- Consider Fertility Preservation: For men who want to delay parenthood or anticipate potential future fertility issues, fertility preservation options such as sperm freezing can offer peace of mind.
In conclusion, the biological clock exists for men and can cause male infertility through factors such as decreased sperm quality, increased risk of genetic abnormalities and reduced sexual function with age. Adopting a healthy lifestyle, undergoing regular fertility tests, seeking medical advice and considering fertility preservation are vital steps for addressing concerns related to male infertility. Understanding and addressing male infertility is crucial for couples striving to conceive and build families.
At Apollo Fertility, we understand the challenges and concerns surrounding fertility. Our renowned clinics offer comprehensive evaluations and personalised treatment options for both men and women. Whether you're considering IVF procedure, IUI treatment, or fertility preservation, our expert team of fertility specialists is here to support and guide you. Schedule a visit with us today and embark on your journey towards parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-13
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-13 01:12:46
[updatedDate] => 2024-03-13 01:14:37
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

Do Men Have Biological Clocks — What Is a Biological Clock?
March 13, 2024When it comes to the topic of fertility, discussions often revolve aro...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 463
[blogcat_id] => 8
[blog_title] => Varicocele — Causes, Symptoms & Diagnosis
[metaTitle] => Understanding and Treating Varicocele
[metaDescription] => Learn about the causes, symptoms and diagnosis of varicocele and how couples dealing with the issue can seek treatment for varicocele.
[metaKeywords] =>
[seo_url] => varicocele-causes-symptoms-diagnosis
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710208903varicocele-causes-symptoms-&-diagnosis.webp
[blog_text] => Varicocele is a common condition affecting males but often individuals are unaware about it or how it can affect fertility. It is a prevalent condition that can have a significant impact on male fertility and in this blog, we will explore varicocele in detail — from its causes and symptoms to its diagnosis and treatment options.
What is Varicocele?
Varicocele is a condition characterised by the enlargement of the veins within the scrotum. These veins are responsible for draining blood from the testicles and when they become dilated or swollen, it can affect the quality and quantity of sperm produced. Varicoceles are most commonly found on the left side of the scrotum, although they can occur on both sides.
Causes of Varicocele
The exact cause of varicocele remains unknown. However, it is believed to be primarily caused by faulty valves within the veins that regulate blood flow. This leads to blood pooling in the veins, resulting in their enlargement. Other factors that may contribute to the development of varicocele include hormonal imbalances and genetic predisposition.
Symptoms of Varicocele
In many cases, varicoceles do not cause noticeable symptoms and are only discovered during routine physical examinations or fertility evaluations. However, some men may experience symptoms such as:
- A dull ache or discomfort in the scrotum.
- Swelling or bulging veins in the scrotum.
- Testicular atrophy (shrinkage) on the affected side.
- Fertility issues, including low sperm count or poor sperm quality.
Diagnosis of Varicocele
If you suspect that you may have a varicocele or are experiencing fertility issues, it is essential to consult with a fertility specialist. During the initial consultation, your fertility doctor will take a detailed medical history and perform a physical examination. They may also recommend the following diagnostic tests:
- Doppler Ultrasound: This non-invasive imaging test uses sound waves to create images of blood flow in the scrotum, allowing your fertility doctor to visualise any abnormalities in the veins.
- Semen Analysis: A semen analysis measures various parameters such as sperm count, motility and morphology. This test helps determine if varicocele is impacting sperm quality.
- Hormone Testing: Hormone levels, including testosterone and follicle-stimulating hormone (FSH), may be tested to assess overall reproductive health.
Treatment Options
The treatment for varicocele depends on several factors, including symptom severity, impact on fertility and personal preferences. The two primary treatment options are:
- Conservative Management: If the varicocele is not causing significant symptoms or affecting fertility, your fertility doctor may recommend conservative management strategies such as wearing supportive underwear or making lifestyle changes that promote overall testicular health.
- Surgical Intervention: If varicocele has significantly caused male infertility or severe discomfort, surgical intervention may be necessary. The most common procedure to treat varicoceles is called varicocelectomy, where the surgeon ligates or closes off the affected veins to redirect blood flow.
In conclusion, varicocele is a common condition affecting males and can significantly impact male infertility. Awareness of its existence and its effects on fertility is essential. Therefore, consulting with a fertility specialist is crucial for diagnosis and exploring treatment options. Whether through conservative management or surgical intervention, addressing varicocele can improve fertility outcomes for individuals experiencing symptoms or fertility issues related to male infertility.
At Apollo Fertility, we understand how challenging and emotionally taxing fertility issues can be. Our team of experienced fertility specialists is here to guide you through every step of your journey towards parenthood. Schedule a consultation with us to explore your options and find the right treatment path for you.
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-12 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-12 02:01:43 [updatedDate] => 2024-03-12 02:02:46 [ip_address] => 49.205.116.233 ) [_oldAttributes:yii\db\BaseActiveRecord:private] => Array ( [blog_id] => 463 [blogcat_id] => 8 [blog_title] => Varicocele — Causes, Symptoms & Diagnosis [metaTitle] => Understanding and Treating Varicocele [metaDescription] => Learn about the causes, symptoms and diagnosis of varicocele and how couples dealing with the issue can seek treatment for varicocele. [metaKeywords] => [seo_url] => varicocele-causes-symptoms-diagnosis [city_id] => [city_name] => [language_id] => 1 [blog_image] => blog-images/1710208903varicocele-causes-symptoms-&-diagnosis.webp [blog_text] =>Varicocele is a common condition affecting males but often individuals are unaware about it or how it can affect fertility. It is a prevalent condition that can have a significant impact on male fertility and in this blog, we will explore varicocele in detail — from its causes and symptoms to its diagnosis and treatment options.
What is Varicocele?
Varicocele is a condition characterised by the enlargement of the veins within the scrotum. These veins are responsible for draining blood from the testicles and when they become dilated or swollen, it can affect the quality and quantity of sperm produced. Varicoceles are most commonly found on the left side of the scrotum, although they can occur on both sides.
Causes of Varicocele
The exact cause of varicocele remains unknown. However, it is believed to be primarily caused by faulty valves within the veins that regulate blood flow. This leads to blood pooling in the veins, resulting in their enlargement. Other factors that may contribute to the development of varicocele include hormonal imbalances and genetic predisposition.
Symptoms of Varicocele
In many cases, varicoceles do not cause noticeable symptoms and are only discovered during routine physical examinations or fertility evaluations. However, some men may experience symptoms such as:
- A dull ache or discomfort in the scrotum.
- Swelling or bulging veins in the scrotum.
- Testicular atrophy (shrinkage) on the affected side.
- Fertility issues, including low sperm count or poor sperm quality.
Diagnosis of Varicocele
If you suspect that you may have a varicocele or are experiencing fertility issues, it is essential to consult with a fertility specialist. During the initial consultation, your fertility doctor will take a detailed medical history and perform a physical examination. They may also recommend the following diagnostic tests:
- Doppler Ultrasound: This non-invasive imaging test uses sound waves to create images of blood flow in the scrotum, allowing your fertility doctor to visualise any abnormalities in the veins.
- Semen Analysis: A semen analysis measures various parameters such as sperm count, motility and morphology. This test helps determine if varicocele is impacting sperm quality.
- Hormone Testing: Hormone levels, including testosterone and follicle-stimulating hormone (FSH), may be tested to assess overall reproductive health.
Treatment Options
The treatment for varicocele depends on several factors, including symptom severity, impact on fertility and personal preferences. The two primary treatment options are:
- Conservative Management: If the varicocele is not causing significant symptoms or affecting fertility, your fertility doctor may recommend conservative management strategies such as wearing supportive underwear or making lifestyle changes that promote overall testicular health.
- Surgical Intervention: If varicocele has significantly caused male infertility or severe discomfort, surgical intervention may be necessary. The most common procedure to treat varicoceles is called varicocelectomy, where the surgeon ligates or closes off the affected veins to redirect blood flow.
In conclusion, varicocele is a common condition affecting males and can significantly impact male infertility. Awareness of its existence and its effects on fertility is essential. Therefore, consulting with a fertility specialist is crucial for diagnosis and exploring treatment options. Whether through conservative management or surgical intervention, addressing varicocele can improve fertility outcomes for individuals experiencing symptoms or fertility issues related to male infertility.
At Apollo Fertility, we understand how challenging and emotionally taxing fertility issues can be. Our team of experienced fertility specialists is here to guide you through every step of your journey towards parenthood. Schedule a consultation with us to explore your options and find the right treatment path for you.
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-12 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-12 02:01:43 [updatedDate] => 2024-03-12 02:02:46 [ip_address] => 49.205.116.233 ) [_related:yii\db\BaseActiveRecord:private] => Array ( ) [_relationsDependencies:yii\db\BaseActiveRecord:private] => Array ( ) [_errors:yii\base\Model:private] => [_validators:yii\base\Model:private] => [_scenario:yii\base\Model:private] => default [_events:yii\base\Component:private] => Array ( ) [_eventWildcards:yii\base\Component:private] => Array ( ) [_behaviors:yii\base\Component:private] => Array ( ) )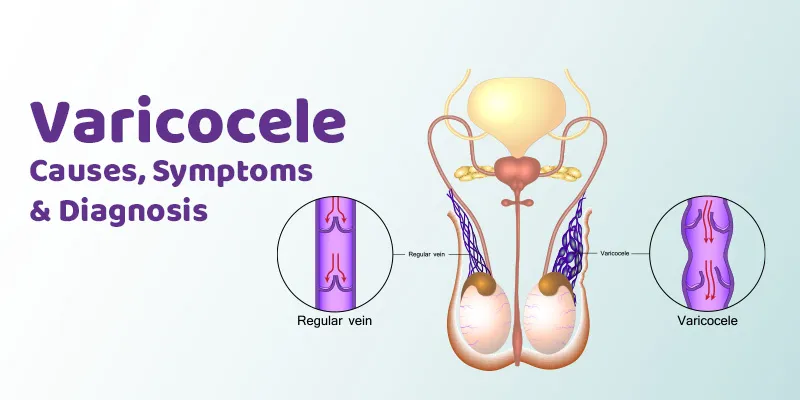
Varicocele — Causes, Symptoms & Diagnosis
March 12, 2024Varicocele is a common condition affecting males but often individuals...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 462
[blogcat_id] => 11
[blog_title] => Intracytoplasmic Sperm Injection (ICSI): Should You Opt for It?
[metaTitle] => Is ICSI The Right Choice For You?
[metaDescription] => Discover what ICSI is and whether it's the right treatment option for you. Learn about the process, success rates, and considerations before making a decision.
[metaKeywords] =>
[seo_url] => intracytoplasmic-sperm-injection-icsi-should-you-opt-for-it
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710133037intracytoplasmic-sperm-injection-(icsi)-should-you-opt-for-it.webp
[blog_text] => If you and your partner have been struggling with fertility issues, you may have come across various treatment options, including ICSI. But what exactly is ICSI, and is it the right choice for you? In this blog, we will explore the benefits, considerations and success rates of ICSI to help you make an informed decision on your path to parenthood.
What is ICSI?
ICSI is a specialised form of in vitro fertilisation (IVF) that addresses male infertility by directly injecting a single sperm into an egg. This procedure helps overcome challenges such as low sperm count, poor sperm motility or abnormal sperm shape. By bypassing natural barriers to fertilisation, ICSI increases the chances of successful fertilisation and subsequent pregnancy.
Benefits of ICSI
- Increased chances of fertilisation: ICSI offers hope to couples who have been struggling with male infertility factors. By directly injecting a healthy sperm into the egg, it improves the chances of successful fertilisation.
- Individualised approach: Unlike the traditional IVF procedure, where multiple sperm are introduced to an egg in a dish, ICSI allows for a more precise selection process. Your fertility doctor or embryologist can choose the best quality sperm for injection, increasing the likelihood of embryo development.
- Treatment for severe male infertility: ICSI can successfully treat severe male infertility issues such as low sperm count or abnormal sperm shape that may hinder natural fertilisation.
- Genetic testing: ICSI also allows for preimplantation genetic testing, which can help identify and select embryos free from certain genetic conditions or chromosomal abnormalities.
Considerations for ICSI
While ICSI offers several benefits, it's essential to consider certain factors before opting for this procedure:
- Cost: ICSI is a more specialised technique compared to the traditional IVF procedure, and it may be more expensive as a result. It is important to discuss the financial aspect with your fertility doctor and ensure you have a clear understanding of the costs involved.
- Ethical considerations: Some individuals may have ethical concerns about the selection process involved in ICSI. It is crucial to have open conversations with your partner and fertility doctor to address any concerns you may have.
- Limited sperm sample: In some cases, there may be a limited number of viable sperm available for injection. This could be due to low sperm count or poor sperm quality. Your fertility specialist will assess the suitability of ICSI based on the available sample.
- No guarantee of success: While ICSI can significantly improve the chances of fertilisation, it does not guarantee pregnancy. It is important to manage expectations and understand that multiple factors contribute to successful conception and pregnancy.
Success rates of ICSI
The success rates of ICSI vary depending on several factors, including the age of the woman, the quality of the eggs and sperm and overall health factors. According to studies conducted in India, the success rates for ICSI can range from 30% to 50%, with higher success rates observed in younger women and couples without additional fertility issues.
In conclusion, ICSI can be a viable option for couples dealing with male infertility factors. However, it's crucial to consult with a fertility specialist who can assess your specific situation and guide you through the decision-making process. If you think ICSI may be the right choice for you and your partner, reach out to Apollo Fertility, a renowned brand in the field of healthcare that offers comprehensive fertility treatments and supports couples on their journey to parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-11
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-11 04:54:11
[updatedDate] => 2024-03-11 05:03:54
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 462
[blogcat_id] => 11
[blog_title] => Intracytoplasmic Sperm Injection (ICSI): Should You Opt for It?
[metaTitle] => Is ICSI The Right Choice For You?
[metaDescription] => Discover what ICSI is and whether it's the right treatment option for you. Learn about the process, success rates, and considerations before making a decision.
[metaKeywords] =>
[seo_url] => intracytoplasmic-sperm-injection-icsi-should-you-opt-for-it
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1710133037intracytoplasmic-sperm-injection-(icsi)-should-you-opt-for-it.webp
[blog_text] => If you and your partner have been struggling with fertility issues, you may have come across various treatment options, including ICSI. But what exactly is ICSI, and is it the right choice for you? In this blog, we will explore the benefits, considerations and success rates of ICSI to help you make an informed decision on your path to parenthood.
What is ICSI?
ICSI is a specialised form of in vitro fertilisation (IVF) that addresses male infertility by directly injecting a single sperm into an egg. This procedure helps overcome challenges such as low sperm count, poor sperm motility or abnormal sperm shape. By bypassing natural barriers to fertilisation, ICSI increases the chances of successful fertilisation and subsequent pregnancy.
Benefits of ICSI
- Increased chances of fertilisation: ICSI offers hope to couples who have been struggling with male infertility factors. By directly injecting a healthy sperm into the egg, it improves the chances of successful fertilisation.
- Individualised approach: Unlike the traditional IVF procedure, where multiple sperm are introduced to an egg in a dish, ICSI allows for a more precise selection process. Your fertility doctor or embryologist can choose the best quality sperm for injection, increasing the likelihood of embryo development.
- Treatment for severe male infertility: ICSI can successfully treat severe male infertility issues such as low sperm count or abnormal sperm shape that may hinder natural fertilisation.
- Genetic testing: ICSI also allows for preimplantation genetic testing, which can help identify and select embryos free from certain genetic conditions or chromosomal abnormalities.
Considerations for ICSI
While ICSI offers several benefits, it's essential to consider certain factors before opting for this procedure:
- Cost: ICSI is a more specialised technique compared to the traditional IVF procedure, and it may be more expensive as a result. It is important to discuss the financial aspect with your fertility doctor and ensure you have a clear understanding of the costs involved.
- Ethical considerations: Some individuals may have ethical concerns about the selection process involved in ICSI. It is crucial to have open conversations with your partner and fertility doctor to address any concerns you may have.
- Limited sperm sample: In some cases, there may be a limited number of viable sperm available for injection. This could be due to low sperm count or poor sperm quality. Your fertility specialist will assess the suitability of ICSI based on the available sample.
- No guarantee of success: While ICSI can significantly improve the chances of fertilisation, it does not guarantee pregnancy. It is important to manage expectations and understand that multiple factors contribute to successful conception and pregnancy.
Success rates of ICSI
The success rates of ICSI vary depending on several factors, including the age of the woman, the quality of the eggs and sperm and overall health factors. According to studies conducted in India, the success rates for ICSI can range from 30% to 50%, with higher success rates observed in younger women and couples without additional fertility issues.
In conclusion, ICSI can be a viable option for couples dealing with male infertility factors. However, it's crucial to consult with a fertility specialist who can assess your specific situation and guide you through the decision-making process. If you think ICSI may be the right choice for you and your partner, reach out to Apollo Fertility, a renowned brand in the field of healthcare that offers comprehensive fertility treatments and supports couples on their journey to parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-11
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-11 04:54:11
[updatedDate] => 2024-03-11 05:03:54
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)
-should-you-opt-for-it.webp)
Intracytoplasmic Sperm Injection (ICSI): Should You Opt for It?
March 11, 2024If you and your partner have been struggling with fertility issues, yo...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 461
[blogcat_id] => 5
[blog_title] => Can Endometrial Polyps Affect Fertility?
[metaTitle] => The Effect of Endometrial Polyps on Fertility
[metaDescription] => Are you struggling to conceive? Learn about the impact of endometrial polyps on fertility, the symptoms to watch for, and the available treatment options.
[metaKeywords] =>
[seo_url] => can-endometrial-polyps-affect-fertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709964770can-endometrial-polyps-affect-fertility.webp
[blog_text] => For couples trying to conceive, navigating the world of fertility can be overwhelming. There are numerous factors that can affect fertility, including endometrial polyps. In this blog, we will explore the link between endometrial polyps and fertility, discuss the symptoms to watch for, and highlight available treatment options.
What are endometrial polyps?
Endometrial polyps are growths that originate in the lining of the uterus, also known as the endometrium. These polyps are typically noncancerous and can vary in size, ranging from a few millimetres to several centimetres. While they can occur at any age, they are more common in women who are in their 40s or 50s.
The impact of endometrial polyps on fertility
Endometrial polyps can have an impact on fertility. The presence of these growths can interfere with implantation and pregnancy by altering the uterine environment. Endometrial polyps may also affect sperm movement within the uterus, making it more difficult for fertilisation to occur.
Furthermore, endometrial polyps can lead to irregular menstrual cycles and heavy or prolonged periods. These factors can make it challenging to track ovulation accurately and time intercourse effectively.
Symptoms of endometrial polyps
While some women with endometrial polyps may not experience any symptoms, others may notice:
- Irregular menstrual bleeding, including heavy or prolonged periods.
- Vaginal bleeding between periods.
- Infertility or difficulty conceiving.
- Pelvic pain or discomfort.
It is important to remember that these symptoms can also be indicative of other gynaecological conditions. If you are experiencing any of these symptoms, it is essential to consult with a fertility specialist, who may suggest fertility tests, for an accurate diagnosis.
How are endometrial polyps diagnosed?
If you suspect you have endometrial polyps or are experiencing fertility issues, your doctor may recommend a thorough evaluation and fertility tests. This evaluation may include:
- Pelvic examination: Your doctor will conduct a physical examination to check for any abnormalities.
- Transvaginal ultrasound: This imaging technique allows the doctor to visualise the uterus and detect the presence of polyps.
- Hysteroscopy: During this procedure, a thin, lighted tube is inserted into the uterus to directly examine the uterine lining and remove any polyps if necessary. Hysteroscopy is considered the gold standard for diagnosing and treating endometrial polyps.
Treatment options for endometrial polyps
The treatment for endometrial polyps depends on various factors, including their size, symptoms and whether or not you are trying to conceive. Treatment options may include:
- Observation: In some cases, small endometrial polyps that are not causing any symptoms may be monitored by your fertility doctor without immediate intervention.
- Medications: Your fertility specialist could prescribe hormonal medications, such as oral contraceptives or progestin-releasing intrauterine devices (IUDs), to help shrink or prevent further growth of endometrial polyps.
- Surgical removal: If the polyps are causing symptoms or affecting fertility, hysteroscopic surgery may be recommended. This minimally invasive procedure allows for the removal of polyps while preserving the uterus.
By addressing endometrial polyps, you can improve your chances of conceiving naturally or increase the success rates of fertility treatments like IVF procedure or IUI procedure. Consulting with a fertility specialist is crucial to determine the most appropriate treatment plan for your specific situation.
At Apollo Fertility, we understand the challenges you may be facing on your fertility journey. Our team of experienced fertility specialists provides comprehensive care and guidance tailored to your individual needs. If you have concerns about endometrial polyps or require assistance with fertility tests or treatments, schedule a consultation today and take the first step towards realising your dream of parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-09
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-09 06:06:38
[updatedDate] => 2024-03-09 06:12:50
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 461
[blogcat_id] => 5
[blog_title] => Can Endometrial Polyps Affect Fertility?
[metaTitle] => The Effect of Endometrial Polyps on Fertility
[metaDescription] => Are you struggling to conceive? Learn about the impact of endometrial polyps on fertility, the symptoms to watch for, and the available treatment options.
[metaKeywords] =>
[seo_url] => can-endometrial-polyps-affect-fertility
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709964770can-endometrial-polyps-affect-fertility.webp
[blog_text] => For couples trying to conceive, navigating the world of fertility can be overwhelming. There are numerous factors that can affect fertility, including endometrial polyps. In this blog, we will explore the link between endometrial polyps and fertility, discuss the symptoms to watch for, and highlight available treatment options.
What are endometrial polyps?
Endometrial polyps are growths that originate in the lining of the uterus, also known as the endometrium. These polyps are typically noncancerous and can vary in size, ranging from a few millimetres to several centimetres. While they can occur at any age, they are more common in women who are in their 40s or 50s.
The impact of endometrial polyps on fertility
Endometrial polyps can have an impact on fertility. The presence of these growths can interfere with implantation and pregnancy by altering the uterine environment. Endometrial polyps may also affect sperm movement within the uterus, making it more difficult for fertilisation to occur.
Furthermore, endometrial polyps can lead to irregular menstrual cycles and heavy or prolonged periods. These factors can make it challenging to track ovulation accurately and time intercourse effectively.
Symptoms of endometrial polyps
While some women with endometrial polyps may not experience any symptoms, others may notice:
- Irregular menstrual bleeding, including heavy or prolonged periods.
- Vaginal bleeding between periods.
- Infertility or difficulty conceiving.
- Pelvic pain or discomfort.
It is important to remember that these symptoms can also be indicative of other gynaecological conditions. If you are experiencing any of these symptoms, it is essential to consult with a fertility specialist, who may suggest fertility tests, for an accurate diagnosis.
How are endometrial polyps diagnosed?
If you suspect you have endometrial polyps or are experiencing fertility issues, your doctor may recommend a thorough evaluation and fertility tests. This evaluation may include:
- Pelvic examination: Your doctor will conduct a physical examination to check for any abnormalities.
- Transvaginal ultrasound: This imaging technique allows the doctor to visualise the uterus and detect the presence of polyps.
- Hysteroscopy: During this procedure, a thin, lighted tube is inserted into the uterus to directly examine the uterine lining and remove any polyps if necessary. Hysteroscopy is considered the gold standard for diagnosing and treating endometrial polyps.
Treatment options for endometrial polyps
The treatment for endometrial polyps depends on various factors, including their size, symptoms and whether or not you are trying to conceive. Treatment options may include:
- Observation: In some cases, small endometrial polyps that are not causing any symptoms may be monitored by your fertility doctor without immediate intervention.
- Medications: Your fertility specialist could prescribe hormonal medications, such as oral contraceptives or progestin-releasing intrauterine devices (IUDs), to help shrink or prevent further growth of endometrial polyps.
- Surgical removal: If the polyps are causing symptoms or affecting fertility, hysteroscopic surgery may be recommended. This minimally invasive procedure allows for the removal of polyps while preserving the uterus.
By addressing endometrial polyps, you can improve your chances of conceiving naturally or increase the success rates of fertility treatments like IVF procedure or IUI procedure. Consulting with a fertility specialist is crucial to determine the most appropriate treatment plan for your specific situation.
At Apollo Fertility, we understand the challenges you may be facing on your fertility journey. Our team of experienced fertility specialists provides comprehensive care and guidance tailored to your individual needs. If you have concerns about endometrial polyps or require assistance with fertility tests or treatments, schedule a consultation today and take the first step towards realising your dream of parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-09
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-09 06:06:38
[updatedDate] => 2024-03-09 06:12:50
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)
Can Endometrial Polyps Affect Fertility?
March 9, 2024For couples trying to conceive, navigating the world of fertility can ...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 460
[blogcat_id] => 18
[blog_title] => Demystifying PCOS
[metaTitle] => Understanding PCOS: Its Causes, Symptoms and Treatment Options
[metaDescription] => Learn about PCOS, its causes, symptoms, and available treatment options to manage this condition effectively and improve your chances of conception.
[metaKeywords] =>
[seo_url] => demystifying-pcos
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709964789demystifying-pcos.webp
[blog_text] => Polycystic Ovary Syndrome (PCOS) affects millions of women worldwide. It is a complex hormonal disorder that can have significant implications for fertility. If you have been diagnosed with PCOS or suspect you may have it, you're not alone.
This blog aims to demystify PCOS by providing accurate information and shedding light on the challenges it presents.
What is PCOS?
PCOS is a hormonal imbalance that affects the ovaries. Women with PCOS often have enlarged ovaries with small cysts on the outer edges. The exact cause of PCOS remains unknown, but it is believed to be a combination of genetic and environmental factors.
Common Symptoms of PCOS
PCOS manifests differently in each woman, but some common symptoms include:
- Irregular periods: Women with PCOS often experience infrequent, irregular or prolonged menstrual cycles.
- Excess hair growth: Due to increased levels of testosterone, women with PCOS may develop excessive hair growth on their face, chest, back, or abdomen.
- Acne: Hormonal imbalances associated with PCOS can contribute to persistent acne breakouts.
- Weight gain: Many women with PCOS struggle with weight gain or find it difficult to lose weight due to insulin resistance.
- Infertility: PCOS is one of the leading causes of female infertility due to irregular ovulation or anovulation (lack of ovulation).
Impact of PCOs on Fertility
PCOS can significantly impact fertility due to hormonal imbalances that interfere with ovulation. In some cases, women with PCOS may not ovulate regularly or may not ovulate at all. Without regular ovulation, it becomes challenging to conceive naturally.
Treatment Options for PCOS
The treatment for PCOS aims to manage symptoms and restore hormonal balance. Lifestyle changes such as maintaining a healthy weight, exercising regularly and following a balanced diet can help improve symptoms and regulate ovulation. In some cases, medication may be prescribed to regulate hormones and induce ovulation.
For individuals experiencing difficulties conceiving due to PCOS, fertility treatments like IUI (Intrauterine Insemination) or IVF procedure (In Vitro Fertilisation) can offer hope. These procedures can help increase the chances of pregnancy by bypassing the challenges posed by irregular ovulation.
What is IUI Treatment?
IUI treatment is a fertility procedure that involves placing sperm directly into the uterus during the woman's fertile window. This procedure can increase the chances of fertilisation by bringing sperm closer to the egg. IUI treatment is often recommended for couples with unexplained infertility or when there are mild male infertility issues.
What is IVF Procedure?
IVF procedure is a more advanced fertility treatment that involves retrieving eggs from the ovaries and fertilising them with sperm in a laboratory. The resulting embryos are then transferred back into the uterus. IVF procedure is suitable for individuals with more complex fertility issues, including severe male infertility or blocked fallopian tubes.
In summary, PCOS presents significant challenges for millions of women worldwide, particularly in the realm of fertility. By demystifying PCOS and exploring treatment options such as lifestyle adjustments, medication, and fertility treatments like IUI procedure and IVF procedure, individuals diagnosed with PCOS can find hope and guidance in navigating their fertility journey.
At Apollo Fertility, we understand the challenges associated with PCOS and the impact it can have on your fertility journey. Our team of experienced fertility specialists provides personalised care, offering a range of treatments tailored to your needs. Take the first step towards achieving your dreams of parenthood by scheduling a consultation at Apollo Fertility today.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-08
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-09 06:02:17
[updatedDate] => 2024-03-09 06:13:09
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 460
[blogcat_id] => 18
[blog_title] => Demystifying PCOS
[metaTitle] => Understanding PCOS: Its Causes, Symptoms and Treatment Options
[metaDescription] => Learn about PCOS, its causes, symptoms, and available treatment options to manage this condition effectively and improve your chances of conception.
[metaKeywords] =>
[seo_url] => demystifying-pcos
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709964789demystifying-pcos.webp
[blog_text] => Polycystic Ovary Syndrome (PCOS) affects millions of women worldwide. It is a complex hormonal disorder that can have significant implications for fertility. If you have been diagnosed with PCOS or suspect you may have it, you're not alone.
This blog aims to demystify PCOS by providing accurate information and shedding light on the challenges it presents.
What is PCOS?
PCOS is a hormonal imbalance that affects the ovaries. Women with PCOS often have enlarged ovaries with small cysts on the outer edges. The exact cause of PCOS remains unknown, but it is believed to be a combination of genetic and environmental factors.
Common Symptoms of PCOS
PCOS manifests differently in each woman, but some common symptoms include:
- Irregular periods: Women with PCOS often experience infrequent, irregular or prolonged menstrual cycles.
- Excess hair growth: Due to increased levels of testosterone, women with PCOS may develop excessive hair growth on their face, chest, back, or abdomen.
- Acne: Hormonal imbalances associated with PCOS can contribute to persistent acne breakouts.
- Weight gain: Many women with PCOS struggle with weight gain or find it difficult to lose weight due to insulin resistance.
- Infertility: PCOS is one of the leading causes of female infertility due to irregular ovulation or anovulation (lack of ovulation).
Impact of PCOs on Fertility
PCOS can significantly impact fertility due to hormonal imbalances that interfere with ovulation. In some cases, women with PCOS may not ovulate regularly or may not ovulate at all. Without regular ovulation, it becomes challenging to conceive naturally.
Treatment Options for PCOS
The treatment for PCOS aims to manage symptoms and restore hormonal balance. Lifestyle changes such as maintaining a healthy weight, exercising regularly and following a balanced diet can help improve symptoms and regulate ovulation. In some cases, medication may be prescribed to regulate hormones and induce ovulation.
For individuals experiencing difficulties conceiving due to PCOS, fertility treatments like IUI (Intrauterine Insemination) or IVF procedure (In Vitro Fertilisation) can offer hope. These procedures can help increase the chances of pregnancy by bypassing the challenges posed by irregular ovulation.
What is IUI Treatment?
IUI treatment is a fertility procedure that involves placing sperm directly into the uterus during the woman's fertile window. This procedure can increase the chances of fertilisation by bringing sperm closer to the egg. IUI treatment is often recommended for couples with unexplained infertility or when there are mild male infertility issues.
What is IVF Procedure?
IVF procedure is a more advanced fertility treatment that involves retrieving eggs from the ovaries and fertilising them with sperm in a laboratory. The resulting embryos are then transferred back into the uterus. IVF procedure is suitable for individuals with more complex fertility issues, including severe male infertility or blocked fallopian tubes.
In summary, PCOS presents significant challenges for millions of women worldwide, particularly in the realm of fertility. By demystifying PCOS and exploring treatment options such as lifestyle adjustments, medication, and fertility treatments like IUI procedure and IVF procedure, individuals diagnosed with PCOS can find hope and guidance in navigating their fertility journey.
At Apollo Fertility, we understand the challenges associated with PCOS and the impact it can have on your fertility journey. Our team of experienced fertility specialists provides personalised care, offering a range of treatments tailored to your needs. Take the first step towards achieving your dreams of parenthood by scheduling a consultation at Apollo Fertility today.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-08
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-09 06:02:17
[updatedDate] => 2024-03-09 06:13:09
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

Demystifying PCOS
March 8, 2024Polycystic Ovary Syndrome (PCOS) affects millions of women worldwide. ...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 459
[blogcat_id] => 5
[blog_title] => What To Know About Subfertility and How to Increase the Odds of Conception
[metaTitle] => Understanding Subfertility and the Chances to Boost Conception
[metaDescription] => what-to-know-about-subfertility-and-how-to-increase-the-odds-of-conceptionStruggling to conceive? Learn about subfertility, its causes and effective strategies to increase your odds of getting pregnant.
[metaKeywords] =>
[seo_url] => what-to-know-about-subfertility-and-how-to-increase-the-odds-of-conception
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709964814what-to-know-about-subfertility-and-how-to-increase-the-odds-of-conception.webp
[blog_text] => Are you dreaming of starting a family but finding it difficult to conceive? You are not alone. Many couples face challenges when trying to have a baby. In medical terms, this condition is called subfertility. It can be a source of stress and frustration, but with the right knowledge and professional guidance from fertility specialists, there is hope. In this blog, we will explore what subfertility is, its causes, and how you can increase your odds of conception.
Understanding Subfertility
Subfertility refers to a reduced ability to conceive within a reasonable time frame. It differs from infertility, which means the inability to conceive altogether. Couples who have been actively trying to get pregnant for more than a year without success may be considered subfertile.
Causes of Subfertility
Subfertility can have various underlying causes, affecting both female and male fertility. It is important to remember that fertility issues can arise from either partner or sometimes a combination of factors. Some common causes include:
- Hormonal Imbalances: Irregular ovulation or problems with hormone production can hinder conception.
- Fallopian Tube Blockage: Blockages in the fallopian tubes prevent the sperm from reaching the egg or the fertilised egg from implanting in the uterus.
- PCOS (Polycystic Ovary Syndrome): PCOS is a hormonal disorder that affects ovulation and can lead to irregular periods or even absence of menstruation.
- Male Factors: Male infertility due to low sperm count, poor sperm quality or blockages in the reproductive system can also contribute to subfertility.
How to Increase the Odds of Conception
While subfertility can be challenging, there are several strategies and treatments available that can increase your chances of getting pregnant:
- Fertility Tests: It is crucial to undergo comprehensive fertility tests to identify any underlying issues. These fertility tests evaluate hormone levels, ovulation, sperm count and other factors that affect female and male fertility.
- Lifestyle Changes: Adopting a healthy lifestyle can positively impact you female and male fertility. Maintain a balanced diet, engage in regular exercise, manage stress and avoid smoking and excessive alcohol consumption.
- Timed Intercourse: Understanding your menstrual cycle and timing intercourse during your most fertile days can maximise the chances of conception. Ovulation prediction kits or tracking basal body temperature can help determine the best timing.
- ART (Assisted Reproductive Techniques): In cases where natural conception is not possible, assisted reproductive techniques such as IUI treatment (Intrauterine Insemination) or IVF treatment (In Vitro Fertilisation) may be recommended by your fertility doctor. These procedures enhance the chances of fertilisation and Implantation.
In conclusion, subfertility presents challenges for couples aspiring to start a family, but it is not an obstacle that cannot be overcome. Understanding the causes of subfertility and seeking professional guidance from fertility specialists are crucial steps towards achieving conception. Through fertility tests, lifestyle adjustments, timed intercourse and assisted reproductive techniques, there is hope for couples navigating the journey of subfertility.
At Apollo Fertility, our experienced team of fertility specialists provides comprehensive evaluations, innovative treatments and unwavering support throughout your fertility journey. Contact us today to schedule a consultation and take the first step towards realising your dream of starting or expanding your family.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-07
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-09 05:57:47
[updatedDate] => 2024-03-09 06:13:34
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 459
[blogcat_id] => 5
[blog_title] => What To Know About Subfertility and How to Increase the Odds of Conception
[metaTitle] => Understanding Subfertility and the Chances to Boost Conception
[metaDescription] => what-to-know-about-subfertility-and-how-to-increase-the-odds-of-conceptionStruggling to conceive? Learn about subfertility, its causes and effective strategies to increase your odds of getting pregnant.
[metaKeywords] =>
[seo_url] => what-to-know-about-subfertility-and-how-to-increase-the-odds-of-conception
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709964814what-to-know-about-subfertility-and-how-to-increase-the-odds-of-conception.webp
[blog_text] => Are you dreaming of starting a family but finding it difficult to conceive? You are not alone. Many couples face challenges when trying to have a baby. In medical terms, this condition is called subfertility. It can be a source of stress and frustration, but with the right knowledge and professional guidance from fertility specialists, there is hope. In this blog, we will explore what subfertility is, its causes, and how you can increase your odds of conception.
Understanding Subfertility
Subfertility refers to a reduced ability to conceive within a reasonable time frame. It differs from infertility, which means the inability to conceive altogether. Couples who have been actively trying to get pregnant for more than a year without success may be considered subfertile.
Causes of Subfertility
Subfertility can have various underlying causes, affecting both female and male fertility. It is important to remember that fertility issues can arise from either partner or sometimes a combination of factors. Some common causes include:
- Hormonal Imbalances: Irregular ovulation or problems with hormone production can hinder conception.
- Fallopian Tube Blockage: Blockages in the fallopian tubes prevent the sperm from reaching the egg or the fertilised egg from implanting in the uterus.
- PCOS (Polycystic Ovary Syndrome): PCOS is a hormonal disorder that affects ovulation and can lead to irregular periods or even absence of menstruation.
- Male Factors: Male infertility due to low sperm count, poor sperm quality or blockages in the reproductive system can also contribute to subfertility.
How to Increase the Odds of Conception
While subfertility can be challenging, there are several strategies and treatments available that can increase your chances of getting pregnant:
- Fertility Tests: It is crucial to undergo comprehensive fertility tests to identify any underlying issues. These fertility tests evaluate hormone levels, ovulation, sperm count and other factors that affect female and male fertility.
- Lifestyle Changes: Adopting a healthy lifestyle can positively impact you female and male fertility. Maintain a balanced diet, engage in regular exercise, manage stress and avoid smoking and excessive alcohol consumption.
- Timed Intercourse: Understanding your menstrual cycle and timing intercourse during your most fertile days can maximise the chances of conception. Ovulation prediction kits or tracking basal body temperature can help determine the best timing.
- ART (Assisted Reproductive Techniques): In cases where natural conception is not possible, assisted reproductive techniques such as IUI treatment (Intrauterine Insemination) or IVF treatment (In Vitro Fertilisation) may be recommended by your fertility doctor. These procedures enhance the chances of fertilisation and Implantation.
In conclusion, subfertility presents challenges for couples aspiring to start a family, but it is not an obstacle that cannot be overcome. Understanding the causes of subfertility and seeking professional guidance from fertility specialists are crucial steps towards achieving conception. Through fertility tests, lifestyle adjustments, timed intercourse and assisted reproductive techniques, there is hope for couples navigating the journey of subfertility.
At Apollo Fertility, our experienced team of fertility specialists provides comprehensive evaluations, innovative treatments and unwavering support throughout your fertility journey. Contact us today to schedule a consultation and take the first step towards realising your dream of starting or expanding your family.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-07
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-09 05:57:47
[updatedDate] => 2024-03-09 06:13:34
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

What To Know About Subfertility and How to Increase the Odds of Conception
March 7, 2024Are you dreaming of starting a family but finding it difficult to conc...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 458
[blogcat_id] => 8
[blog_title] => How To Improve the Quality of Egg for IVF Naturally
[metaTitle] => How to Naturally Improve Eggs Quality for IVF
[metaDescription] => Have you wondered if there are ways to naturally improve the quality of eggs for IVF procedure? Read on to discover expert tips to optimise your chances of success.
[metaKeywords] =>
[seo_url] => how-to-improve-the-quality-of-egg-for-ivf-naturally
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709705590how-to-improve-the-quality-of-egg-for-ivf-naturally.webp
[blog_text] => In vitro fertilisation (IVF) can be an incredibly hopeful and transformative journey for couples seeking to start a family. However, one of the key factors that contribute to the success of IVF procedure is the quality of eggs. For individuals considering IVF, it's important to explore every opportunity to improve egg quality naturally. In this blog post, we will discuss some strategies and lifestyle changes that can help enhance the quality of eggs for IVF procedure.
Prioritise a Nutrient-Rich Diet
A balanced diet plays a crucial role in optimising fertility. To improve egg quality, focus on consuming a fertility diet, that is nutrient-rich foods which are high in antioxidants, vitamins and minerals. Include plenty of fresh fruits and vegetables, whole grains, lean proteins and healthy fats in your diet. Some specific fertility foods include leafy greens, berries, nuts and seeds, avocados and fatty fish like salmon.
Maintain a Healthy Weight
Maintaining a healthy weight is essential for reproductive health. Both overweight and underweight individuals may experience hormonal imbalances that can affect egg quality. Aim to achieve a healthy Body Mass Index (BMI) by adopting a well-balanced, fertility diet and incorporating regular exercise into your routine.
Engage in Regular Physical Activity
Regular exercise has been shown to have positive effects on fertility. Engaging in moderate-intensity exercises like brisk walking, swimming or yoga can improve blood circulation to the ovaries and promote overall reproductive health. However, avoid excessive exercise as it may have adverse effects on fertility.
Manage Stress Levels
Stress can negatively impact reproductive health and egg quality. Incorporating stress management techniques such as meditation, deep breathing exercises, yoga or engaging in hobbies can help reduce stress levels. Prioritise self-care and take time for activities that bring you joy and relaxation.
Get Sufficient Sleep
Adequate sleep is crucial for hormonal balance and overall well-being. Aim for 7-8 hours of quality sleep every night to support optimal egg quality.
Limit Alcohol and Caffeine Intake
Excessive alcohol and caffeine consumption have been linked to decreased fertility and poor egg quality. It is advisable to limit alcohol intake and moderate your caffeine consumption during IVF procedure.
Quit Smoking
Smoking has been shown to have detrimental effects on fertility, including decreased egg quality. If you're a smoker, quitting is one of the best steps you can take to improve your chances of successful IVF procedure.
Consider Supplements
Consult with your fertility doctor about incorporating certain supplements into your routine that may support egg quality. Some commonly recommended supplements include Coenzyme Q10 (CoQ10), Omega-3 fatty acids, Vitamin D and antioxidants like Vitamin C and E. However, it is important that you speak to your fertility specialist before beginning any medication before and during the IVF procedure.
Stay Hydrated
Drinking an adequate amount of water throughout the day is essential for maintaining optimal health, including reproductive health. Aim for at least 8-10 glasses of water daily to stay hydrated.
Seek Expert Guidance
Every individual's fertility journey is unique, and it is important to seek guidance from a qualified fertility specialist or reproductive endocrinologist. They can assess your specific situation, conduct necessary tests, and provide personalised recommendations based on your medical history.
Improving egg quality naturally takes time, patience and dedication. While these strategies can enhance your chances of successful IVF procedure, it is essential to work closely with a fertility specialist who can guide you through the process.
To explore fertility treatment options, consult with our expert team at Apollo Fertility. Visit our website to schedule a consultation today.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-06
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-06 06:13:10
[updatedDate] => 2024-03-06 06:13:10
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 458
[blogcat_id] => 8
[blog_title] => How To Improve the Quality of Egg for IVF Naturally
[metaTitle] => How to Naturally Improve Eggs Quality for IVF
[metaDescription] => Have you wondered if there are ways to naturally improve the quality of eggs for IVF procedure? Read on to discover expert tips to optimise your chances of success.
[metaKeywords] =>
[seo_url] => how-to-improve-the-quality-of-egg-for-ivf-naturally
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709705590how-to-improve-the-quality-of-egg-for-ivf-naturally.webp
[blog_text] => In vitro fertilisation (IVF) can be an incredibly hopeful and transformative journey for couples seeking to start a family. However, one of the key factors that contribute to the success of IVF procedure is the quality of eggs. For individuals considering IVF, it's important to explore every opportunity to improve egg quality naturally. In this blog post, we will discuss some strategies and lifestyle changes that can help enhance the quality of eggs for IVF procedure.
Prioritise a Nutrient-Rich Diet
A balanced diet plays a crucial role in optimising fertility. To improve egg quality, focus on consuming a fertility diet, that is nutrient-rich foods which are high in antioxidants, vitamins and minerals. Include plenty of fresh fruits and vegetables, whole grains, lean proteins and healthy fats in your diet. Some specific fertility foods include leafy greens, berries, nuts and seeds, avocados and fatty fish like salmon.
Maintain a Healthy Weight
Maintaining a healthy weight is essential for reproductive health. Both overweight and underweight individuals may experience hormonal imbalances that can affect egg quality. Aim to achieve a healthy Body Mass Index (BMI) by adopting a well-balanced, fertility diet and incorporating regular exercise into your routine.
Engage in Regular Physical Activity
Regular exercise has been shown to have positive effects on fertility. Engaging in moderate-intensity exercises like brisk walking, swimming or yoga can improve blood circulation to the ovaries and promote overall reproductive health. However, avoid excessive exercise as it may have adverse effects on fertility.
Manage Stress Levels
Stress can negatively impact reproductive health and egg quality. Incorporating stress management techniques such as meditation, deep breathing exercises, yoga or engaging in hobbies can help reduce stress levels. Prioritise self-care and take time for activities that bring you joy and relaxation.
Get Sufficient Sleep
Adequate sleep is crucial for hormonal balance and overall well-being. Aim for 7-8 hours of quality sleep every night to support optimal egg quality.
Limit Alcohol and Caffeine Intake
Excessive alcohol and caffeine consumption have been linked to decreased fertility and poor egg quality. It is advisable to limit alcohol intake and moderate your caffeine consumption during IVF procedure.
Quit Smoking
Smoking has been shown to have detrimental effects on fertility, including decreased egg quality. If you're a smoker, quitting is one of the best steps you can take to improve your chances of successful IVF procedure.
Consider Supplements
Consult with your fertility doctor about incorporating certain supplements into your routine that may support egg quality. Some commonly recommended supplements include Coenzyme Q10 (CoQ10), Omega-3 fatty acids, Vitamin D and antioxidants like Vitamin C and E. However, it is important that you speak to your fertility specialist before beginning any medication before and during the IVF procedure.
Stay Hydrated
Drinking an adequate amount of water throughout the day is essential for maintaining optimal health, including reproductive health. Aim for at least 8-10 glasses of water daily to stay hydrated.
Seek Expert Guidance
Every individual's fertility journey is unique, and it is important to seek guidance from a qualified fertility specialist or reproductive endocrinologist. They can assess your specific situation, conduct necessary tests, and provide personalised recommendations based on your medical history.
Improving egg quality naturally takes time, patience and dedication. While these strategies can enhance your chances of successful IVF procedure, it is essential to work closely with a fertility specialist who can guide you through the process.
To explore fertility treatment options, consult with our expert team at Apollo Fertility. Visit our website to schedule a consultation today.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-06
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-06 06:13:10
[updatedDate] => 2024-03-06 06:13:10
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

How To Improve the Quality of Egg for IVF Naturally
March 6, 2024In vitro fertilisation (IVF) can be an incredibly hopeful and transfor...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 457
[blogcat_id] => 8
[blog_title] => Exploring AMH and Its Relevance in Women's Health
[metaTitle] => Understanding AMH Testing and Its Importance for Women's Fertility
[metaDescription] => Curious about AMH testing? Learn what AMH is, why it is important for women's fertility, and how it can help in planning for pregnancy.
[metaKeywords] =>
[seo_url] => exploring-amh-and-its-relevance-in-womens-health
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709705337exploring-amh-and-its-relevance-in-womens-health.webp
[blog_text] => As many couples embark on their journey to start a family, they may encounter various challenges along the way. One such challenge is understanding the factors that affect fertility and the different tests available to evaluate fertility potential. One such test that has gained popularity in recent years is anti-Mullerian hormone (AMH) testing. In this article, we will delve into the details of AMH testing, its importance, and how it can assist couples on their journey towards parenthood.
What is AMH?
AMH is a hormone produced by small follicles in the ovaries. It acts as a marker of a woman's ovarian reserve, which refers to the quantity and quality of eggs remaining in her ovaries. The level of AMH in the blood can provide insights into the number of viable eggs a woman has and estimate her reproductive potential.
Importance of AMH Testing for Women
AMH testing can be valuable in several scenarios:
- Assessing Ovarian Reserve: As mentioned earlier, AMH levels can indicate a woman's ovarian reserve. This information helps in creating an individualised treatment plan to optimise outcomes.
- Predicting Response to Assisted Reproductive Technologies: For women undergoing IVF procedures, knowing their AMH levels can help predict their response to ovarian stimulation medications. This prediction allows fertility doctors to tailor the dosage of medications, improving the chances of success in each cycle.
- Monitoring Fertility Preservation: For women considering fertility preservation, such as egg freezing, AMH testing can help assess their ovarian reserve before undergoing the procedure.
- Identifying Premature Ovarian Insufficiency (POI): POI refers to a condition where a woman's ovaries stop functioning before the age of 40. AMH testing can aid in diagnosing POI early.
- Planning for Natural Conception: Although AMH levels alone cannot determine a woman's chances of natural conception, they provide insights into her reproductive potential.
In conclusion, AMH testing is a valuable tool in assessing a woman's ovarian reserve and optimising fertility treatment outcomes. If you are planning for pregnancy or considering fertility preservation options, consult with an experienced fertility specialist who can guide you through the process. At Apollo Fertility, we offer comprehensive fertility services and personalised care to help couples achieve their dream of parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-05
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-06 06:08:57
[updatedDate] => 2024-03-06 06:10:25
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 457
[blogcat_id] => 8
[blog_title] => Exploring AMH and Its Relevance in Women's Health
[metaTitle] => Understanding AMH Testing and Its Importance for Women's Fertility
[metaDescription] => Curious about AMH testing? Learn what AMH is, why it is important for women's fertility, and how it can help in planning for pregnancy.
[metaKeywords] =>
[seo_url] => exploring-amh-and-its-relevance-in-womens-health
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709705337exploring-amh-and-its-relevance-in-womens-health.webp
[blog_text] => As many couples embark on their journey to start a family, they may encounter various challenges along the way. One such challenge is understanding the factors that affect fertility and the different tests available to evaluate fertility potential. One such test that has gained popularity in recent years is anti-Mullerian hormone (AMH) testing. In this article, we will delve into the details of AMH testing, its importance, and how it can assist couples on their journey towards parenthood.
What is AMH?
AMH is a hormone produced by small follicles in the ovaries. It acts as a marker of a woman's ovarian reserve, which refers to the quantity and quality of eggs remaining in her ovaries. The level of AMH in the blood can provide insights into the number of viable eggs a woman has and estimate her reproductive potential.
Importance of AMH Testing for Women
AMH testing can be valuable in several scenarios:
- Assessing Ovarian Reserve: As mentioned earlier, AMH levels can indicate a woman's ovarian reserve. This information helps in creating an individualised treatment plan to optimise outcomes.
- Predicting Response to Assisted Reproductive Technologies: For women undergoing IVF procedures, knowing their AMH levels can help predict their response to ovarian stimulation medications. This prediction allows fertility doctors to tailor the dosage of medications, improving the chances of success in each cycle.
- Monitoring Fertility Preservation: For women considering fertility preservation, such as egg freezing, AMH testing can help assess their ovarian reserve before undergoing the procedure.
- Identifying Premature Ovarian Insufficiency (POI): POI refers to a condition where a woman's ovaries stop functioning before the age of 40. AMH testing can aid in diagnosing POI early.
- Planning for Natural Conception: Although AMH levels alone cannot determine a woman's chances of natural conception, they provide insights into her reproductive potential.
In conclusion, AMH testing is a valuable tool in assessing a woman's ovarian reserve and optimising fertility treatment outcomes. If you are planning for pregnancy or considering fertility preservation options, consult with an experienced fertility specialist who can guide you through the process. At Apollo Fertility, we offer comprehensive fertility services and personalised care to help couples achieve their dream of parenthood.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-05
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-06 06:08:57
[updatedDate] => 2024-03-06 06:10:25
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

Exploring AMH and Its Relevance in Women's Health
March 5, 2024As many couples embark on their journey to start a family, they may en...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 456
[blogcat_id] => 8
[blog_title] => Understanding Nonobstructive Azoospermia: Causes and Solutions
[metaTitle] => Nonobstructive Azoospermia Explored: What You Need to Know
[metaDescription] => Explore the causes, diagnostic methods, and treatment options available for nonobstructive azoospermia to help you overcome this condition and achieve your dream of having a child.
[metaKeywords] =>
[seo_url] => understanding-nonobstructive-azoospermia-causes-and-solutions
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709554157understanding-nonobstructive-azoospermia-causes-and-solutions.webp
[blog_text] => Parenthood is a dream many couples share. The journey to conceive can be exciting, but it can also present challenges along the way. One such challenge is nonobstructive azoospermia, a condition where the male partner produces no sperm in their semen. In this article, we will break down nonobstructive azoospermia, including its causes, diagnosis methods, and treatment options to help you navigate through this fertility issue.
Causes of Nonobstructive Azoospermia
Some of the common causes of nonobstructive azoospermia include:
- Hormonal Imbalances: Hormonal imbalances such as low levels of testosterone or high levels of follicle-stimulating hormone (FSH).
- Genetic Abnormalities: Genetic abnormalities such as Klinefelter syndrome or Y-chromosome microdeletions.
- Varicocele: A varicocele is a condition where the veins in the scrotum become enlarged, leading to decreased sperm production.
- Testicular Dysfunction: Conditions that impact testicular function, such as mumps orchitis, testicular trauma, or radiation therapy, can lead to nonobstructive azoospermia.
- Medications: Some medications, such as chemotherapy drugs or testosterone replacement therapy, can negatively impact sperm production.
Diagnosing Nonobstructive Azoospermia
The following male fertility tests are commonly used to diagnose nonobstructive azoospermia:
- Semen Analysis: A semen analysis is performed to evaluate the quality and quantity of sperm in the semen sample.
- Hormone Testing: Blood tests can assess hormone levels, including testosterone, FSH, and luteinising hormone (LH), to determine if there are any hormonal imbalances.
- Genetic Testing: Genetic testing may be recommended to identify any genetic abnormalities that could be causing nonobstructive azoospermia.
- Testicular Biopsy: In some cases, a testicular biopsy may be recommended to evaluate the presence or absence of sperm within the testicles.
Treatment Options for Nonobstructive Azoospermia
Treatment options for nonobstructive azoospermia depend on the underlying cause and individual circumstances.
- In some cases, addressing hormonal imbalances or treating underlying medical conditions may improve sperm production.
- However, for individuals with severe sperm production issues, assisted reproductive technologies such as in vitro fertilisation (IVF) or intracytoplasmic sperm injection may be recommended.
- In cases where nonobstructive azoospermia is a result of chemotherapy or radiation therapy, fertility preservation techniques such as sperm freezing before treatment can provide future options for conception.
In conclusion, nonobstructive azoospermia presents unique challenges in achieving pregnancy. However, with advancements in reproductive medicine and the expertise of fertility specialists at Apollo Fertility, there are viable treatment options available. If you or your partner are facing nonobstructive azoospermia, we encourage you to schedule a consultation with our experienced team to explore personalised solutions tailored to your needs.
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-04 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-04 12:09:17 [updatedDate] => 2024-03-04 12:09:17 [ip_address] => 49.205.116.233 ) [_oldAttributes:yii\db\BaseActiveRecord:private] => Array ( [blog_id] => 456 [blogcat_id] => 8 [blog_title] => Understanding Nonobstructive Azoospermia: Causes and Solutions [metaTitle] => Nonobstructive Azoospermia Explored: What You Need to Know [metaDescription] => Explore the causes, diagnostic methods, and treatment options available for nonobstructive azoospermia to help you overcome this condition and achieve your dream of having a child. [metaKeywords] => [seo_url] => understanding-nonobstructive-azoospermia-causes-and-solutions [city_id] => [city_name] => [language_id] => 1 [blog_image] => blog-images/1709554157understanding-nonobstructive-azoospermia-causes-and-solutions.webp [blog_text] =>Parenthood is a dream many couples share. The journey to conceive can be exciting, but it can also present challenges along the way. One such challenge is nonobstructive azoospermia, a condition where the male partner produces no sperm in their semen. In this article, we will break down nonobstructive azoospermia, including its causes, diagnosis methods, and treatment options to help you navigate through this fertility issue.
Causes of Nonobstructive Azoospermia
Some of the common causes of nonobstructive azoospermia include:
- Hormonal Imbalances: Hormonal imbalances such as low levels of testosterone or high levels of follicle-stimulating hormone (FSH).
- Genetic Abnormalities: Genetic abnormalities such as Klinefelter syndrome or Y-chromosome microdeletions.
- Varicocele: A varicocele is a condition where the veins in the scrotum become enlarged, leading to decreased sperm production.
- Testicular Dysfunction: Conditions that impact testicular function, such as mumps orchitis, testicular trauma, or radiation therapy, can lead to nonobstructive azoospermia.
- Medications: Some medications, such as chemotherapy drugs or testosterone replacement therapy, can negatively impact sperm production.
Diagnosing Nonobstructive Azoospermia
The following male fertility tests are commonly used to diagnose nonobstructive azoospermia:
- Semen Analysis: A semen analysis is performed to evaluate the quality and quantity of sperm in the semen sample.
- Hormone Testing: Blood tests can assess hormone levels, including testosterone, FSH, and luteinising hormone (LH), to determine if there are any hormonal imbalances.
- Genetic Testing: Genetic testing may be recommended to identify any genetic abnormalities that could be causing nonobstructive azoospermia.
- Testicular Biopsy: In some cases, a testicular biopsy may be recommended to evaluate the presence or absence of sperm within the testicles.
Treatment Options for Nonobstructive Azoospermia
Treatment options for nonobstructive azoospermia depend on the underlying cause and individual circumstances.
- In some cases, addressing hormonal imbalances or treating underlying medical conditions may improve sperm production.
- However, for individuals with severe sperm production issues, assisted reproductive technologies such as in vitro fertilisation (IVF) or intracytoplasmic sperm injection may be recommended.
- In cases where nonobstructive azoospermia is a result of chemotherapy or radiation therapy, fertility preservation techniques such as sperm freezing before treatment can provide future options for conception.
In conclusion, nonobstructive azoospermia presents unique challenges in achieving pregnancy. However, with advancements in reproductive medicine and the expertise of fertility specialists at Apollo Fertility, there are viable treatment options available. If you or your partner are facing nonobstructive azoospermia, we encourage you to schedule a consultation with our experienced team to explore personalised solutions tailored to your needs.
[search_keywords] => [blog_status] => Active [published_date] => 2024-03-04 [createdBy] => 1 [updatedBy] => 1 [createdDate] => 2024-03-04 12:09:17 [updatedDate] => 2024-03-04 12:09:17 [ip_address] => 49.205.116.233 ) [_related:yii\db\BaseActiveRecord:private] => Array ( ) [_relationsDependencies:yii\db\BaseActiveRecord:private] => Array ( ) [_errors:yii\base\Model:private] => [_validators:yii\base\Model:private] => [_scenario:yii\base\Model:private] => default [_events:yii\base\Component:private] => Array ( ) [_eventWildcards:yii\base\Component:private] => Array ( ) [_behaviors:yii\base\Component:private] => Array ( ) )
Understanding Nonobstructive Azoospermia: Causes and Solutions
March 4, 2024Parenthood is a dream many couples share. The journey to conceive can ...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 455
[blogcat_id] => 14
[blog_title] => Myth vs. Reality in IVF: Debunking Misconceptions
[metaTitle] => Understanding IVF: Common Myths and the Truth Behind Them
[metaDescription] => Discover the truth behind common misconceptions surrounding IVF. Find answers to your questions about IVF in this informative article.
[metaKeywords] =>
[seo_url] => myth-vs-reality-in-ivf-debunking-misconceptions
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709291595myth-vs-reality-in-ivf-debunking-misconceptions.webp
[blog_text] => If you're considering in vitro fertilisation (IVF) as a fertility treatment option, it's important to separate fact from fiction about the IVF procedure. There are many myths and misconceptions surrounding IVF that can cause unnecessary worry and confusion. In this article, we will debunk some of the most common myths about IVF and provide you with accurate information to help you make informed decisions.
Myth 1: IVF is the Only Option for Infertility
Fact: Although IVF is a popular option, it is not the only treatment available for infertility. Before recommending an IVF procedure, fertility specialists thoroughly evaluate each individual's specific circumstances, exploring other less invasive options such as medication, lifestyle changes, or intrauterine insemination (IUI).
Myth 2: IVF is Only for Women With Fertility Problems
Fact: Both men and women can experience fertility issues. In some cases, male infertility or a combination of male and female factors may necessitate the use of IVF.
Myth 3: IVF is Always Successful
Fact: Although the IVF procedure has significantly improved pregnancy rates for couples struggling with infertility, it is not a guaranteed solution. Success rates can vary depending on several factors including age, underlying health conditions, and the quality of both eggs and sperm.
Myth 4: IVF is Extremely Painful
Fact: The IVF procedure is not as painful as many believe. The egg retrieval process is typically done under sedation, so you will not experience any discomfort during the procedure. Some women may experience mild cramping and bloating afterward, but these symptoms are temporary and can be managed with over-the-counter pain relievers.
Myth 5: IVF Increases the Risk of Multiple Pregnancies
Fact: In the past, IVF treatments did have a higher risk of multiple pregnancies due to the transfer of multiple embryos. However, advancements in technology and a better understanding of embryo selection have significantly reduced this risk. Today, most fertility clinics follow a single-embryo transfer policy, where only one carefully selected embryo is transferred to minimise the chances of multiple pregnancies while maintaining high success rates.
In conclusion, it's important to separate myths from facts when considering IVF as a fertility treatment option. IVF is a highly effective and safe procedure that has helped thousands of couples achieve their dream of parenthood. If you're considering IVF or have any questions about the process, we encourage you to reach out to Apollo Fertility, a renowned brand in the field of healthcare in India, for expert guidance and personalised care.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-01
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-01 11:13:15
[updatedDate] => 2024-03-01 11:13:15
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 455
[blogcat_id] => 14
[blog_title] => Myth vs. Reality in IVF: Debunking Misconceptions
[metaTitle] => Understanding IVF: Common Myths and the Truth Behind Them
[metaDescription] => Discover the truth behind common misconceptions surrounding IVF. Find answers to your questions about IVF in this informative article.
[metaKeywords] =>
[seo_url] => myth-vs-reality-in-ivf-debunking-misconceptions
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709291595myth-vs-reality-in-ivf-debunking-misconceptions.webp
[blog_text] => If you're considering in vitro fertilisation (IVF) as a fertility treatment option, it's important to separate fact from fiction about the IVF procedure. There are many myths and misconceptions surrounding IVF that can cause unnecessary worry and confusion. In this article, we will debunk some of the most common myths about IVF and provide you with accurate information to help you make informed decisions.
Myth 1: IVF is the Only Option for Infertility
Fact: Although IVF is a popular option, it is not the only treatment available for infertility. Before recommending an IVF procedure, fertility specialists thoroughly evaluate each individual's specific circumstances, exploring other less invasive options such as medication, lifestyle changes, or intrauterine insemination (IUI).
Myth 2: IVF is Only for Women With Fertility Problems
Fact: Both men and women can experience fertility issues. In some cases, male infertility or a combination of male and female factors may necessitate the use of IVF.
Myth 3: IVF is Always Successful
Fact: Although the IVF procedure has significantly improved pregnancy rates for couples struggling with infertility, it is not a guaranteed solution. Success rates can vary depending on several factors including age, underlying health conditions, and the quality of both eggs and sperm.
Myth 4: IVF is Extremely Painful
Fact: The IVF procedure is not as painful as many believe. The egg retrieval process is typically done under sedation, so you will not experience any discomfort during the procedure. Some women may experience mild cramping and bloating afterward, but these symptoms are temporary and can be managed with over-the-counter pain relievers.
Myth 5: IVF Increases the Risk of Multiple Pregnancies
Fact: In the past, IVF treatments did have a higher risk of multiple pregnancies due to the transfer of multiple embryos. However, advancements in technology and a better understanding of embryo selection have significantly reduced this risk. Today, most fertility clinics follow a single-embryo transfer policy, where only one carefully selected embryo is transferred to minimise the chances of multiple pregnancies while maintaining high success rates.
In conclusion, it's important to separate myths from facts when considering IVF as a fertility treatment option. IVF is a highly effective and safe procedure that has helped thousands of couples achieve their dream of parenthood. If you're considering IVF or have any questions about the process, we encourage you to reach out to Apollo Fertility, a renowned brand in the field of healthcare in India, for expert guidance and personalised care.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-03-01
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-03-01 11:13:15
[updatedDate] => 2024-03-01 11:13:15
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

Myth vs. Reality in IVF: Debunking Misconceptions
March 1, 2024If you're considering in vitro fertilisation (IVF) as a fertility ...
backend\modules\blogs\models\Blogs Object
(
[categoriesList] =>
[citiesList] =>
[langList] =>
[blogFaqs] =>
[_attributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 454
[blogcat_id] => 5
[blog_title] => Why And When Should You Leave Your Ob-Gyn for a Fertility Doctor?
[metaTitle] => Why And When Should You Leave Your Ob-Gyn for a Fertility Doctor?
[metaDescription] => Are you struggling with fertility issues? Learn when it might be time to consult a fertility specialist and how they can help you on your journey to parenthood.
[metaKeywords] =>
[seo_url] => why-and-when-should-you-leave-your-ob-gyn-for-a-fertility-doctor
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709207266why-and-when-should-you-leave-your-ob-gyn-for-a-fertility-doctor.webp
[blog_text] => If you feel like you've exhausted all your options with your current obstetrician-gynaecologist (Ob-Gyn), it may be time to consider consulting a fertility specialist. A fertility specialist can provide specialised care and treatment for couples facing fertility challenges. In this blog, we will explore the reasons why and when you should leave your Ob-Gyn for a fertility doctor.
Why Should you Consider Consulting a Fertility Specialist?
Facing infertility challenges can be emotionally draining, and it's important to remember that you are not alone. Seeking the expertise of a fertility specialist can offer numerous benefits.
Specialised knowledge and experience
Fertility doctors have extensive training and experience in diagnosing and treating various fertility issues. They understand the complexities of reproductive health and are up-to-date with the latest advancements in fertility tests and treatments.
Comprehensive evaluation
A fertility specialist will conduct a thorough evaluation of both partners to identify the underlying causes of infertility. By evaluating both female and male infertility factors, they can develop personalised treatment plans tailored to your specific needs.
Advanced treatment options
Fertility specialists offer a wide range of advanced treatment options such as intrauterine insemination (IUI) and in vitro fertilisation (IVF). These procedures have helped many couples achieve their dream of parenthood.
Emotional support
Dealing with infertility can take an emotional toll on individuals and couples. Fertility specialists are trained to provide compassionate support throughout your journey, offering guidance, counselling, and resources to help you cope with the emotional aspects of infertility.
When is the Right Time to Consult a Fertility Specialist?
While every individual's journey is unique, there are some signs that indicate it may be time to seek the help of a fertility specialist:
- Age-related concerns: If you're a woman over the age of 35 and have been attempting to conceive for six months or more without success, it's recommended to consult a fertility specialist. Age can significantly impact fertility, and early intervention can improve your chances of success.
- Irregular menstrual cycles: If you have irregular periods or experience very light or heavy bleeding, it could be an indication of an underlying hormonal imbalance or other reproductive issues. A fertility specialist can help identify the cause and develop a suitable treatment plan.
- Known reproductive health issues: If you or your partner have known reproductive health issues such as polycystic ovary syndrome (PCOS), endometriosis or previous infertility concerns, consulting with a fertility specialist early on can increase your chances of success.
- Unexplained infertility: If you and your partner have undergone thorough testing with your Ob-Gyn and no clear cause for infertility has been identified, it may be time to consult a fertility specialist who can conduct further investigations and provide a fresh perspective.
Transitioning to a fertility specialist from an Ob-Gyn represents a pivotal step for couples navigating fertility challenges. With specialised expertise, personalised care, and advanced treatments, fertility specialists offer tailored solutions and renewed hope on the path to parenthood.
If you're ready to take the next step in your fertility journey, consider consulting a fertility specialist at Apollo Fertility. With our renowned expertise and compassionate care, we are dedicated to helping couples achieve their dreams of parenthood. Schedule a consultation with our experienced fertility doctors today.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-02-29
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-02-29 11:45:37
[updatedDate] => 2024-02-29 11:47:46
[ip_address] => 49.205.116.233
)
[_oldAttributes:yii\db\BaseActiveRecord:private] => Array
(
[blog_id] => 454
[blogcat_id] => 5
[blog_title] => Why And When Should You Leave Your Ob-Gyn for a Fertility Doctor?
[metaTitle] => Why And When Should You Leave Your Ob-Gyn for a Fertility Doctor?
[metaDescription] => Are you struggling with fertility issues? Learn when it might be time to consult a fertility specialist and how they can help you on your journey to parenthood.
[metaKeywords] =>
[seo_url] => why-and-when-should-you-leave-your-ob-gyn-for-a-fertility-doctor
[city_id] =>
[city_name] =>
[language_id] => 1
[blog_image] => blog-images/1709207266why-and-when-should-you-leave-your-ob-gyn-for-a-fertility-doctor.webp
[blog_text] => If you feel like you've exhausted all your options with your current obstetrician-gynaecologist (Ob-Gyn), it may be time to consider consulting a fertility specialist. A fertility specialist can provide specialised care and treatment for couples facing fertility challenges. In this blog, we will explore the reasons why and when you should leave your Ob-Gyn for a fertility doctor.
Why Should you Consider Consulting a Fertility Specialist?
Facing infertility challenges can be emotionally draining, and it's important to remember that you are not alone. Seeking the expertise of a fertility specialist can offer numerous benefits.
Specialised knowledge and experience
Fertility doctors have extensive training and experience in diagnosing and treating various fertility issues. They understand the complexities of reproductive health and are up-to-date with the latest advancements in fertility tests and treatments.
Comprehensive evaluation
A fertility specialist will conduct a thorough evaluation of both partners to identify the underlying causes of infertility. By evaluating both female and male infertility factors, they can develop personalised treatment plans tailored to your specific needs.
Advanced treatment options
Fertility specialists offer a wide range of advanced treatment options such as intrauterine insemination (IUI) and in vitro fertilisation (IVF). These procedures have helped many couples achieve their dream of parenthood.
Emotional support
Dealing with infertility can take an emotional toll on individuals and couples. Fertility specialists are trained to provide compassionate support throughout your journey, offering guidance, counselling, and resources to help you cope with the emotional aspects of infertility.
When is the Right Time to Consult a Fertility Specialist?
While every individual's journey is unique, there are some signs that indicate it may be time to seek the help of a fertility specialist:
- Age-related concerns: If you're a woman over the age of 35 and have been attempting to conceive for six months or more without success, it's recommended to consult a fertility specialist. Age can significantly impact fertility, and early intervention can improve your chances of success.
- Irregular menstrual cycles: If you have irregular periods or experience very light or heavy bleeding, it could be an indication of an underlying hormonal imbalance or other reproductive issues. A fertility specialist can help identify the cause and develop a suitable treatment plan.
- Known reproductive health issues: If you or your partner have known reproductive health issues such as polycystic ovary syndrome (PCOS), endometriosis or previous infertility concerns, consulting with a fertility specialist early on can increase your chances of success.
- Unexplained infertility: If you and your partner have undergone thorough testing with your Ob-Gyn and no clear cause for infertility has been identified, it may be time to consult a fertility specialist who can conduct further investigations and provide a fresh perspective.
Transitioning to a fertility specialist from an Ob-Gyn represents a pivotal step for couples navigating fertility challenges. With specialised expertise, personalised care, and advanced treatments, fertility specialists offer tailored solutions and renewed hope on the path to parenthood.
If you're ready to take the next step in your fertility journey, consider consulting a fertility specialist at Apollo Fertility. With our renowned expertise and compassionate care, we are dedicated to helping couples achieve their dreams of parenthood. Schedule a consultation with our experienced fertility doctors today.
[search_keywords] =>
[blog_status] => Active
[published_date] => 2024-02-29
[createdBy] => 1
[updatedBy] => 1
[createdDate] => 2024-02-29 11:45:37
[updatedDate] => 2024-02-29 11:47:46
[ip_address] => 49.205.116.233
)
[_related:yii\db\BaseActiveRecord:private] => Array
(
)
[_relationsDependencies:yii\db\BaseActiveRecord:private] => Array
(
)
[_errors:yii\base\Model:private] =>
[_validators:yii\base\Model:private] =>
[_scenario:yii\base\Model:private] => default
[_events:yii\base\Component:private] => Array
(
)
[_eventWildcards:yii\base\Component:private] => Array
(
)
[_behaviors:yii\base\Component:private] => Array
(
)
)

Why And When Should You Leave Your Ob-Gyn for a Fertility Doctor?
February 29, 2024If you feel like you've exhausted all your options with your curre...
Categories
- Surgery (5)
- Uncategorised (1)
- Egg Donar (2)
- Egg Health (6)
- Fertility (102)
- Fertility Issues (10)
- Fibroids (1)
- General (15)
- Getting Infertility (2)
- Getting Pregnant (35)
- ICSI (10)
- Infertility (99)
- IUI (14)
- IVF (90)
- Laser Assisted Hatching (3)
- lifestyle (3)
- Ovulation (13)
- PCOS (10)
- pregnancy (14)
- Sperm Donation (5)
- Sperm health (9)
OVULATION CALCULATOR
Request a Call
Thank you